5 mg, 10 mg and 20 mg tablets
lisinopril (as dihydrate)
What Lisinopril Stada is and what it is used for
Lisinopril Stada contains the active substance lisinopril. Lisinopril belongs to a group of medicines called ACE inhibitors. These work by dilating the blood vessels, which makes it easier for the heart to pump blood to different parts of the body. This leads to a decrease in blood pressure.
Lisinopril contained in Lisinopril Stada may also be approved for the treatment of other conditions not mentioned in this product information. Ask your doctor, pharmacist, or other healthcare professionals if you have any further questions, and always follow their instructions.
Lisinopril Stada is used if:
- You have high blood pressure .
- You suffer from heart failure . This means that your heart does not have enough pumping power to transport around the blood as well as before, leading to disease-related symptoms such as fatigue, shortness of breath or swelling in the ankles and feet.
- You have had a heart attack (in this case, Lisinopril Stada is used as a short-term treatment for 6 weeks, within 24 hours).
- You have kidney problems associated with diabetes and high blood pressure .
What you need to know before you use Lisinopril Stada
Do not take Lisinopril Stada
- if you are allergic to lisinopril or to any other medicine belonging to the same group of medicines as lisinopril ( ACE inhibitor ) or to any of the other ingredients of this medicine (listed in section 6)
- if you have previously had an allergic reaction to lisinopril or similar medicines ( ACE inhibitors ) with symptoms such as itching , hives , wheezing or swelling of the hands, throat, mouth or eyelids
- if you or anyone in your family has previously had allergic reactions that have caused difficulty swallowing or breathing, swelling of the hands, feet, ankles, face, lips, tongue or throat ( angioedema ) or if you have had angioedema at any other time
- if you are pregnant and longer than the third month. (it is good to avoid Lisinopril Stada even early in pregnancy – see Pregnancy and breast-feeding)
- if you have diabetes or renal impairment and are being treated with a blood pressure lowering medicine containing aliskiren
- if you have taken or are taking sakubitril / valsartan, a medicine used to treat a type of long-term ( chronic ) heart failure in adults, as it increases the risk of angioedema (rapid swelling under the skin in an area such as the throat).
Warnings and cautions
Talk to your doctor or pharmacist before taking Lisinopril Stada.
- if you are taking any of the following medicines used to treat high blood pressure:
- an angiotensin II receptor blocker (ARB) (also known as sartans – for example valsartan, telmisartan, irbesartan), especially if you have diabetes-related kidney problems
- aliskiren.
Your doctor may need to check your kidney function, blood pressure, and the number of electrolytes (eg potassium ) in your blood at regular intervals.
See also the information under the heading “Do not take Lisinopril Stada”.
Talk to your doctor or pharmacist if you have or have had any illnesses, especially any of the following conditions:
Pregnancy
If you think you may be pregnant or become pregnant during treatment, consult your doctor. Lisinopril Stada is not recommended during early pregnancy and should not be taken if the pregnancy is longer than 3 months, as it may cause serious birth defects if used at that stage, see Pregnancy and breastfeeding.
Low blood pressure
Lisinopril Stada may in rare cases cause low blood pressure, especially at the beginning of treatment.
This occurs more often in patients who:
- are dehydrated or have a salt deficiency, eg during diuretic treatment, low-salt diet, dialysis , diarrhea or vomiting (see also section 2. “Other medicines and Lisinopril Stada” and 4. “Possible side effects”)
- have a severe form of high blood pressure caused by kidney disease (see also section 2. “Other medicines and Lisinopril Stada” and 4. “Possible side effects”)
- have severe heart failure (due to the use of high doses of diuretics, with or without renal impairment)
- have angina or cerebrovascular disease. Lisinopril Stada can cause a heart attack or stroke . These patients need close medical supervision.
If you have an increased risk of a drop in blood pressure, your doctor will monitor you closely, especially at the beginning of treatment. The doctor may also change the dosage.
Severe drop in blood pressure
If you have a sharp drop in blood pressure, lie down. If it persists, you may need medical attention. A temporary drop in blood pressure does not mean that you can not continue treatment with Lisinopril Stada. When your blood pressure has returned to normal, you can take Lisinopril Stada as usual. In some cases, however, it may be necessary to reduce the dose or end the treatment. Talk to your doctor if your blood pressure drops too much or often.
Heart valve and heart muscle diseases
Use caution when using Lisinopril Stada if you suffer from it
- narrowing of the heart valves, which prevents the outflow of blood from the heart
- thickening of the heart muscle.
Inform your doctor about your condition and ask him/her for advice.
Hypersensitivity reactions (allergic reactions) or angioedema
ACE inhibitors (including lisinopril) have in rare cases caused a life-threatening allergic reaction called angioedema. Very rare cases of fatal angioedema have been reported, with swelling of the larynx or tongue causing airway obstruction.
Stop taking Lisinopril Stada immediately and contact your doctor if you experience any symptoms of angioedema, such as:
- swelling of face, arms, legs, lips, tongue and / or throat
- difficulty swallowing
- difficulty breathing
- hives.
You are more likely to get angioedema about
- you are dark-skinned
- you have previously had angioedema , even if it was not caused by an ACE inhibitor (see section “Do not take Lisinopril Stada” above).
If you take any of the following medicines, the risk of angioedema (rapidly developing swelling under the skin in areas such as the throat) may increase:
- racekadotril, a medicine used to treat diarrhea.
- drugs used to prevent rejection of transplanted organs and against cancer (eg temsirolimus, sirolimus, everolimus).
- vildagliptin, a medicine used to treat diabetes .
Fatal anaphylactic (allergic) reactions have occurred in patients who have undergone the following treatments with ACE inhibitors:
Tell your doctor that you are taking Lisinopril Stada if you are taking it at the same time
- hemodialysis
- removal of LDL lipoprotein (a special technique used to remove fat from the blood)
- desensitization treatment, eg against bee or wasp venom.
Ethnic differences
Like other ACE inhibitors, Lisinopril Stada may be less effective in dark-skinned patients. Angioedema is also more common in dark-skinned patients than in light-skinned patients.
Kidney diseases
If you have kidney disease or impaired kidney function, your doctor may need to monitor your potassium and creatinine levels carefully and possibly adjust the dose of lisinopril (see also ‘How to take Lisinopril Stada’).
You should not take Lisinopril Stada if you have recently had a kidney transplant.
Special conditions can affect your kidneys:
- In patients with heart failure , low blood pressure caused by ACE inhibitors may worsen renal function. Acute renal failure , usually transient, has been reported in this case.
- In some patients, who have been treated with ACE inhibitors and at the same time had narrowing of the renal blood vessels (mono- or bilateral renal artery stenosis), an increase in urea and creatinine in the blood has been observed. This is more common in patients with renal impairment. The increases are usually transient when the treatment is stopped.
- Patients also suffer from high blood pressure because of the disease in the renal artery s (renovascular hypertension ) are at greater risk for low blood pressure and kidney failure . These patients should start treatment under close supervision and with low doses and careful dose adjustments. Treatment with diuretics should be discontinued and renal function should be monitored during the first few weeks of treatment with Lisinopril Stada.
- Some patients with high blood pressure without any previous disease of the blood vessels of the kidneys (renovascular disease) have experienced an increase in urea and creatinine in the blood. These increases have usually been small and transient. It is more likely to affect patients who already have impaired kidney function. If this happens, your doctor may reduce your dose or prescribe another medicine for you.
If your kidney function deteriorates, your doctor should evaluate your treatment carefully. He/she may ask you to stop taking Lisinopril Stada.
Liver disease
ACE inhibitors have in rare cases been associated with a condition that begins with yellowing of the skin and whites of the eyes as a result of a blockage of bile from the liver to the intestinal tract (cholestatic jaundice). Thereafter, the process occurs rapidly with cell death in the liver (liver necrosis) and (sometimes) death.
If you develop jaundice, stop taking Lisinopril Stada and contact your doctor immediately. If your doctor notices a change in your liver enzymes, he/she may ask you to stop taking Lisinopril Stada.
Change in the number of blood cells
Changes in blood cell counts have been reported during treatment with ACE inhibitors (see section 4. “Possible side effects”).
These changes can make you more susceptible to infections, bleeding, or the risk of getting bruises. Tell your doctor if you notice any of these symptoms. He/she can check your blood count and possibly ask you to stop treatment, if necessary. Some of these changes disappear after treatment with ACE inhibitors is stopped.
You should be extra careful and ask your doctor for advice:
- If you suffer from a disease of the connective tissue, such as blood, bones or cartilage ( collagen , vascular disease).
- If you are taking any of the following medicines:
- Immunosuppressive drugs (medicines that reduce the activity of the immune system, for example after an organ transplant).
- Allopurinol (for the treatment of gout and high levels of urea in the blood).
- Procainamide (medicine for irregular heartbeat).
This is especially important if your kidneys are not working properly.
Increase in potassium in the blood (hyperkalemia)
You are at increased risk for hyperkalemia if:
- your kidneys are not functioning normally
- you suffer from diabetes mellitus
- you are taking other medicines that are associated with an increase in the level of potassium in your blood.
If you need to take any of the above medicines, your doctor will monitor your blood potassium levels regularly (see section “Other medicines and Lisinopril Stada” below).
Diabetes
If you are taking diabetes medicines that you take by mouth or insulin, your blood sugar levels should be closely monitored during the first month of treatment (see section “Other medicines and Lisinopril Stada” below). The dosage of one of your diabetes medications may need to be adjusted.
Surgery or anesthesia
If you are going to have an operation or dental surgery, tell your doctor or dentist that you are taking Lisinopril Stada before you are given anesthesia.
Lithium
You must tell your doctor if you are taking lithium or medicines containing lithium (used to treat mania or depression). The combination of Lisinopril Stada and lithium is generally not recommended (see section “Other medicines and Lisinopril Stada”).
Other medicines and Lisinopril Stada
Tell your doctor or pharmacist if you are taking, have recently taken, or might take any other medicines.
The effect of the medicine can be affected if it is taken at the same time as other medicines. You must tell your doctor or pharmacist if you are taking, have recently taken, or might take any of the following medicines:
The following drugs may enhance the effects of lisinopril STADA, thereby increasing the risk of low blood pressure ( hypotension ):
- Diuretics ( diuretics ). If you are already taking diuretics, tell your doctor. He / she will inform you to stop the diuretic treatment 2 to 3 days before taking Lisinopril Stada.
- Other antihypertensive drugs.
- Glyceryl nitrate (for the treatment of angina and heart failure ) and other nitrates.
- Other vasodilators (medicines that dilate blood vessels).
- Tricyclic antidepressants (for the treatment of depression).
- Antipsychotics (for the treatment of mental illness / psychosis).
- Anesthetics.
The following medicines may reduce the effect of Lisinopril Stada :
- Non-steroidal anti-inflammatory drugs (painkillers), including acetylsalicylic acid , in doses higher than 3 g per day. Chronic use of these drugs may reduce the antihypertensive effect of Lisinopril Stada. There is also a risk of increased levels of potassium in the blood and deterioration of kidney function, including kidney failure .
- Sympathomimetics (drugs with a stimulating effect that raises blood pressure ).
Lisinopril Stada may affect the effectiveness of the following medicines :
- Drugs that lower blood sugar levels ( insulin and oral diabetes medicines). Risk of hypoglycaemia (low blood sugar), especially at the beginning of treatment and in patients with renal impairment.
- Lithium (used to treat mania or depression). You should not take Lisinopril Stada with lithium. If the combination is necessary, the level of lithium in the blood must be closely monitored. Concomitant treatment with Lisinopril Stada and thiazides (a diuretic) may increase the risk of exposure.
Use of these medicines with Lisinopril Stada may increase the risk of side effects are. These include kidney failure, change in the number of blood cells, hyperkalemia (high levels of potassium in the blood):
- potassium supplements (including salt substitutes), potassium-sparing diuretic agent (diuretic), and other drugs that may increase the amount of potassium in your blood (such as trimethoprim and cotrimoxazole (trimethoprim / sulfamethoxazole) against infection s caused by bacteria, cyclosporine, an immunosuppressive drug which prevents the rejection of transplanted organs; and heparin , a drug used to thin the blood to prevent blood clots).
- use of drugs including gold for injection (for example to treat rheumatism or joint disease) while Lisinopril Stada may increase the risk of a so-called nitritoid reaction (relaxed blood vessels) with symptoms that include redness , malaise, dizziness and drop in blood pressure, which may be serious.
- drugs most commonly used to prevent rejection of transplanted organs (sirolimus, everolimus and other drugs belonging to the group mTOR inhibitors). See section “Warnings and Precautions”.
Your doctor may need to change your dose and/or take other precautions:
If you are taking an angiotensin II receptor blocker (ARB) or aliskiren (see also the information under the headings “Do not take Lisinopril Stada” and “Warnings and precautions”)
Lisinopril Stada with food and drink
Food intake does not affect the uptake of lisinopril. Therefore, you can take Lisinopril Stada with or without food, but try to take a dose at the same time each day.
Pregnancy and breastfeeding
If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Pregnancy
If you think you may be pregnant or become pregnant during treatment, you should contact your doctor. Your doctor will usually suggest that you stop taking Lisinopril before you become pregnant or as soon as you know you are pregnant and will advise you to take another medicine instead of Lisinopril Stada.
Lisinopril Stada is not recommended in early pregnancy and should not be taken if the pregnancy is longer than the third month, as it can cause serious birth defects if used after the third month of pregnancy.
Breast-feeding
Talk to your doctor if you are breastfeeding or about to start breastfeeding. Lisinopril Stada is not recommended during breastfeeding, and your doctor may choose another treatment for you if you wish to breastfeed, especially if your baby is newborn or born prematurely.
Driving and using machines
Your tablets are not likely to affect your ability to drive or use machines. Sometimes, however, they may make you feel dizzy or tired, especially at the beginning of treatment with Lisinopril Stada. Do not drive or use machines until you know you are not affected.
You are responsible for assessing whether you are fit to drive a motor vehicle or perform work that requires sharpened attention. One of the factors that can affect your ability in these respects is the use of drugs due to their effects and/or side effects. Descriptions of these effects and side effects can be found in other sections. Read all the information in this leaflet for guidance. If you are not sure, talk to your doctor or pharmacist.
How to use Lisinopril Stada
Always take this medicine exactly as your doctor has told you. Ask your doctor or pharmacist if you are unsure.
You can take Lisinopril Stada with or without food. Swallow the tablet with a glass of water at one time for a daily dose. Try to take the tablet at the same time each day. Continue to take Lisinopril Stada for as long as your doctor prescribes it.
For Lisinopril Stada 5 mg tablets:
If your doctor has prescribed you to take 1/2 tablet, you will need to split the tablet along the breaker before taking it, by placing it on a hard surface with the breaker facing up. Press with your thumb from above and the tablet will be divided into two halves (see picture).
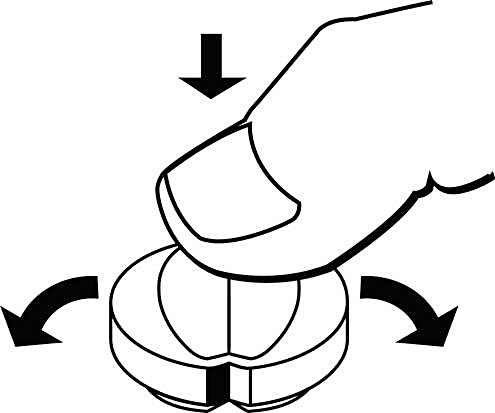
For Lisinopril Stada 10 mg and 20 mg tablets
If your doctor has prescribed you to take 1/2 or 1/4 tablet, you will need to split the tablet along the breaker notches before taking it, by placing it on a hard surface with the breaker notch facing up. Press with your thumb from above and the tablet will be divided into four equal halves (see picture).
The recommended dose depends on the severity of your illness and your patient profile.
The following recommended dose is listed below:
In the high blood pressure
Lisinopril Stada can be used alone or in combination with other antihypertensive medicines.
The usual starting dose is 10 mg once a day. The dose is gradually increased at intervals of at least 2-4 weeks until your blood pressure is effectively controlled.
The usual long-term dosage is 20 mg once daily. Depending on how you respond to treatment, the dose may be increased gradually to a maximum dose of 80 mg once daily.
If you are already taking diuretics, your doctor will ask you to stop taking this treatment 2 to 3 days before you start using Lisinopril Stada. If the diuretic treatment can not be stopped, lisinopril treatment should start with 5 mg once daily. Dose one can then be adjusted according to your blood pressure response. The diuretic treatment may need to be resumed.
If you have kidney problems, you can start treatment at a lower dose. Your doctor will decide on the dosage depending on the severity of your kidney disease. He/she will monitor your values closely, especially at the beginning of treatment (see section “Warnings and Precautions; Kidney Diseases”).
Use for children and adolescents (6 – 16 years)
Dose one is determined by the doctor. The recommended starting dose is 2.5 mg once daily if the baby’s weight is between 20 and 50 kg, 5 mg once daily if the baby weighs more than 50 kg.
The doctor will adjust the daily dose one individually to a maximum of 20 mg daily for children weighing between 20 and 50 kg and 40 mg for children weighing more than 50 kg. Doses above 40 mg are not recommended for use in children.
If your child has kidney problems, your doctor may start with a lower starting dose or increase the dose gradually over a longer time.
In case of heart failure
Lisinopril Stada should be used as adjunctive therapy to another therapy for the treatment of heart failure (for example with diuretics, digitalis, beta-blockers ).
The usual starting dose is 2.5 mg once a day, which should be taken under medical supervision. Dose one will then be increased in increments of no more than 10 mg, at least every two weeks for the treatment of heart failure.
A maximum dose of 35 mg daily should not be exceeded.
Your doctor may adjust your dose based on your clinical response.
After a heart attack
After the recommended treatment (with, for example, anticoagulant, beta-blocker ), the normal starting dose is:
- 5 mg within 24 hours after the heart attack.
- Then 5 mg 24 hours after the first dose .
- Then 10 mg 48 hours after the first dose one, followed by 10 mg once daily.
The usual maintenance dose is 10 mg once daily.
Your doctor may lower your dose if you have low blood pressure or kidney problems.
Treatment should be continued for 6 weeks.
In case of problems in connection with diabetes
The usual starting dose is 10 mg once daily for patients with high blood pressure.
Dose one can, if necessary, be increased to 20 mg once daily.
If you have kidney problems, your dose may need to be adjusted.
Use for children
This medicine should not be given to children under 6 years of age or children with severe kidney problems. Ask your doctor for advice.
Use in the elderly
Elderly people with normal kidney function can take the same dose as normal.
Use in patients with kidney transplants
The use of Lisinopril Stada is not recommended for patients who have had a kidney transplant.
Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
The first or second dose of one of these tablets may make you feel dizzy or faint as a result of a drop in blood pressure. This usually disappears if you lie down.
You should immediately stop taking Lisinopril Stada and tell your doctor if you:
- feels itching or develops severe skin reactions
- have wheezing, difficulty breathing or difficulty swallowing
- may have swollen hands, feet or ankles, face, lips, tongue or throat, or
- gets yellow skin or whites of the eyes.
Common (may affect up to 1 in 10 people):
- dizziness
- headache
- orthostatic effects (including hypotension , in this case a drop in blood pressure in connection with getting up which causes dizziness, fainting or fainting)
- cough
- diarrhea
- vomiting
- problems with renal function ( renal dysfunction ).
Uncommon (may affect up to 1 in 100 people):
- swelling of face, arms, legs, lips, tongue, vocal cords, and / or throat. These are symptoms of an angioneurotic edema , caused by a hypersensitivity reaction ( allergic reaction ) (see section “Warnings and precautions; Hypersensitivity reactions (allergic reactions) or angioedema”)
- changes in mood
- tingling or numbness in the hands or feet ( paresthesias )
- a feeling of dizziness or vertigo ( vertigo )
- taste changes
- sleep disorders
- heart attack (myocardial infarction) or cerebrovascular accident ( stroke ), possibly secondary result of very low blood pressure ( hypotension ) in high risk patients (see “Precautions; Low blood pressure”).
- palpitations ( palpitation )
- fast heartbeat ( tachycardia )
- impaired blood circulation leading to numb and pale hands and feet (Reynaud’s phenomenon)
- swelling and irritation of the nose
- nausea
- abdominal pain
- impaired digestion
- rash
- itching
- impotence
- fatigue
- feeling dull ( asthenia )
- increase in urea in the blood
- increase in creatinine in the blood
- increase in liver enzymes
- high levels of potassium in the blood, which can lead to abnormal heart rhythm ( hyperkalemia ).
Rare (may affect up to 1 in 1,000 people):
- decreased hemoglobin ( red blood cells )
- decreased hematocrit (the proportion of red blood cells in the blood)
- mental confusion
- dry mouth
- hives (utricaria)
- hair loss ( alopecia )
- psoriasis , a skin disease that causes red spots and inflammation of the skin.
- a poisoning condition caused by kidney failure and characterized by accumulation of urea in the blood ( uremia )
- acute renal failure
- breast augmentation in men ( gynecomastia )
- elevated levels of bilirubin in the blood
- low levels of sodium in the blood which can lead to muscle weakness, twitching or abnormal heart rhythm ( hyponatremia )
- increase in a certain hormone that regulates the amount of water in the blood and thus affects the salt balance, e.g. decreased sodium levels, a condition called “inadequate ADH secretion” (SIADH) – symptoms may include confusion, weakness, fatigue, headache, nausea, vomiting and cramps.
Very rare (may affect up to 1 in 10,000 people):
- when a bone marrow does not produce enough blood cells (bone marrow depression)
- decreased number of red blood cells which can make the skin pale and give a feeling of weakness or shortness of breath ( anemia , hemolytic anemia )
- decreased number of red platelets which may increase the risk of bleeding or bruising ( thrombocytopenia )
- low white blood cell count ( leukopenia )
- low number of a special type of white blood cell called neutrophilic granulocytes ( neutropenia )
- sharp decrease in the number of white blood cells which increases the risk of infection ( agranulocytosis , see section “Warnings and precautions; Change in the number of blood cells”)
- enlargement of lymph nodes ( lymphadenopathy )
- autoimmune disease
- low blood sugar ( hypoglycaemia )
- difficulty breathing or wheezing ( bronchospasm )
- sinusitis ( sinusitis )
- inflammation of the pulmonary alveoli caused by allergy (allergic alveolitis)
- accumulation of white blood cells ( eosinophilia ) in the lungs ( eosinophilic pneumonia )
- inflammation of the pancreas which causes severe pain in the abdomen and back ( pancreatitis )
- swelling of the mucous membranes of the intestinal tract (intestinal angioedema )
- inflammation of the liver ( hepatitis ), either hepatocellular or cholecostatic
- yellowing of the skin or whites of the eyes caused by problems with the liver or blood (jaundice, see section “Take special care with Lisinopril Stada; Liver disease”)
- increased sweating
- an autoimmune disease that causes blistering and open sores on the skin ( pemphigus )
- severe disease with blistering of the skin (toxic epidermal necrolysis )
- severe disease with blistering of the skin, mouth, eyes and genitals ( Stevens-Johnson syndrome )
- a skin disease with itchy, pinkish spots ( erythem multiforme)
- decreased / absent urine production (oliguria / anuria)
- symptoms similar to a skin tumor originating in the lymphatic system (an inflammatory response that results in an accumulation of inflammatory cells).
Has been reported (occurs in the unknown number of users):
- depressive symptoms
- fainting ( syncope ).
A collection of symptoms, containing one or more of the following, have been reported: fever, inflammation of the blood vessels, often accompanied by a rash ( vasculitis ), muscle pain ( myalgia ), joint pain ( arthralgia ) / inflammation of the joints ( arthritis ), a positive response to antinuclear antibodies (ANA; a blood test to detect autoimmune diseases), elevated red blood cell sedimentation rate (ESR; a blood test that can detect signs of inflammation in the body), a certain type of white blood cell ( eosinophils ) and a high number of other white blood cells( leukocytes ), skin rash, sensitivity to sunlight ( photosensitivity ) or other skin reactions may occur.
How to store Lisinopril Stada
Keep this medicine out of the sight and reach of children.
Do not store above 30 ° C
Do not use this medicine after the expiry date which is stated on the outer carton and blister. The expiration date is the last day of the specified month. Return all unused medicines to your pharmacy.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
Contents of the pack and other information
Content declaration
- The active substance is lisinopril (as dihydrate). One tablet contains 5 mg, 10 mg or 20 mg lisinopril.
- The other ingredients are calcium hydrogen phosphate dihydrate, anhydrous colloidal silica, magnesium stearate, corn starch, mannitol, pregelatinized corn starch.
What the medicine looks like and contents of the pack
Lisinopril Stada 5 mg tablets
White, round, biconvex tablets with a notch on both sides and the text “5” on one side. Each tablet contains 5.44 mg of lisinopril dihydrate equivalent to 5 mg of lisinopril.
Lisinopril Stada 10 mg tablets
White, round, biconvex tablets with a cross notch on both sides and with the text “10” on one side. Each tablet contains 10.89 mg of lisinopril dihydrate equivalent to 10 mg of lisinopril.
Lisinopril Stada 20 mg tablets
White, round, biconvex tablets with a cross notch on both sides and the text “20” on one side. Each tablet contains 21.78 mg of lisinopril dihydrate equivalent to 20 mg of lisinopril.
The tablets are packed in blister packs of the following sizes:
14, 20, 28, 30, 50, 56, 60, 98, 100, 150, 200, 250, 300, 400, 500 and 1000 tablets
Marketing Authorization Holder and Manufacturer
STADA Arzneimittel AG
Stadastrasse 2-18
61118 Bad Vilbel
Germany
Local representative
STADA Nordic ApS
Marielundvej 46 A
2730 Herlev
Denmark