0.03 mg / 3 mg film-coated tablets
Ethinyl estradiol/drospirenone
1. What Cleosensa is and what it is used for
Cleosensa is a contraceptive ( birth control pill ) and is used to prevent pregnancy.
Each tablet contains a small amount of two different female sex hormones, drospirenone and ethinyl estradiol.
Birth control pills that contain two hormones are called combined birth control pills.
Ethinyl estradiol and drospirenone contained in Cleosensa may also be approved for the treatment of other conditions not mentioned in this product information. Ask your doctor, pharmacist or other healthcare professional if you have any further questions and always follow their instructions.
2. What you need to know before you use Cleosensa
Do not use Cleosensa
| Generally Before you start using Cleosensa, read the information on blood clots in section 2. It is especially important that you read the symptoms of blood clots – see section 2, “Blood clots”. Your doctor will ask some questions about your own and your immediate relatives’ medical history. Your doctor will also measure your blood pressure and also take other tests depending on your situation. This leaflet describes several situations in which you should stop using Cleosensa or when the reliability of Cleosensa may be reduced. Under such circumstances, you should not have sex without using supplemental non-hormonal contraceptives, such as condoms or other barrier methods . Do not use the rhythm method or the temperature method. These methods are not reliable because Cleosensa affects the monthly changes in body temperature and cervical secretions. Like other hormonal contraceptives protect Cleosensa not against HIV – infection( AIDS ) or other sexually transmitted diseases. |
Do not use Cleosensa
Do not use Cleosensa if you have any of the conditions listed below. If you have any of these conditions, tell your doctor. The doctor will discuss what other type of contraception may be more appropriate.
- if you have (or have had) a blood clot in a blood vessel in your legs (deep vein thrombosis , DVT), in your lungs ( pulmonary embolism ) or any other organ
- if you know you have a disease that affects blood clotting – e.g. protein C deficiency, protein S deficiency, antithrombin III deficiency, Factor V Leiden or antiphospholipid antibodies
- if you need to have an operation or if you stay in bed for a long period of time (see section “Blood clots”)
- If you have (or have had) a heart attack or stroke (stroke)
- if you have (or have had) angina (a condition that causes severe chest pain and may be a first sign of a heart attack) or transient ischemic attack ( TIA – transient stroke symptoms)
- if you have any of the following conditions that may increase the risk of blood clots in your arteries:
- severe diabetes with damaged blood vessels
- very high blood pressure
- a very high level of fat in the blood ( cholesterol or triglycerides )
- a condition called hyperhomocysteinemia
- if you have (or have had) a type of migraine called “migraine with aura”
- if you have (or have had) a liver disease and your liver is still not functioning normally
- if your kidneys are not working well ( kidney failure )
- if you have (or have had) a tumor in your liver
- if you have (or have had) or if you suspect breast or genital cancer
- if you have unexplained vaginal bleeding
- if you are allergic to ethinyl estradiol or drospirenone or any of the other ingredients of this medicine (listed in section 6). This can cause itching , rash or swelling.
- if you have hepatitis C and are taking medicines containing ombitasvir / paritaprevir / ritonavir and dasabuvir (see also section “Other medicines and Cleosensa”)
Warnings and cautions
| When should you contact a doctor? Seek medical attention immediatelyif you notice possible signs of a blood clot that may mean you have a blood clot in your leg (ie deep vein thrombosis ), a blood clot in your lung (ie pulmonary embolism ), a heart attack or a stroke (see section “Blood clots” below). For a description of the symptoms of these serious side effects, go to “How to recognize a blood clot”. |
Tell your doctor if any of the following conditions apply to you
In some situations, you need to be especially careful when using Cleosensa or other combined birth control pills , and you may need to be examined regularly by your doctor. Before you start using Cleosensa, tell your doctor if any of the following conditions apply to you. If the condition occurs or worsens when you use Cleosensa, you should also consult a doctor:
- if a close relative has or has had breast cancer
- if you have liver or gallbladder disease
- if you have diabetes
- if you suffer from depression
- if you have Crohn’s disease or ulcerative colitis ( chronic inflammatory bowel disease)
- if you have hemolytic urematic syndrome (HUS – a disorder of blood coagulation that leads to kidney failure )
- if you have sickle cell anemia (a hereditary disease of the red blood cells )
- if you have epilepsy (see also “Other medicines and Cleosensa”)
- if you have systemic lupus erythematosus ( SLE – a disease that affects your natural immune system)
- if you have increased blood fats ( hypertriglyceridemia ) or a hereditary condition. Hypertriglyceridemia has been associated with an increased risk of developing pancreatitis (inflammation of the pancreas)
- if you need to have an operation or stay in bed for a longer period (see section 2 “Blood clots”)
- if you have just given birth, you are at increased risk of getting a blood clot. Ask your doctor how soon after giving birth you can start using Cleosensa
- if you have an inflammation of the veins under the skin (superficial thrombophlebitis )
- if you have varicose veins
- if you have a disease that first appeared during pregnancy or during previous use of sex hormones (eg hearing loss, a blood disease called porphyria , skin rash with blisters during pregnancy (pregnancy herpes), a nerve disease that causes sudden twitching in the body (dance disease) )
- if you have or have had chloasma (a discoloration of the skin, especially on the face or neck, so-called “pregnancy spots”). If you have this, avoid direct sunlight and ultraviolet light.
- If you have hereditary angioedema , estrogen- containing products may cause or worsen the symptoms. Contact a doctor immediately if you experience symptoms such as swelling of the face, tongue and / or throat and / or difficulty swallowing, or hives associated with difficulty breathing.
BLOOD CLOTS
Using combined hormonal contraceptives such as Cleosensa increases the risk of blood clots compared to if you do not use these drugs. In rare cases, a blood clot can block the blood vessels and cause serious problems.
Blood clots can form
- in veins (called venous thrombosis , venous thromboembolism or VTE)
- in arteries (called arterial thrombosis , arterial thromboembolism or ATE).
It is not always possible to fully recover from blood clots. In rare cases, they can have serious lasting effects and, in very rare cases, be fatal.
It is important to remember that the overall risk of a dangerous blood clot due to Cleosensa is small.
HOW TO FEEL A BLOOD CLOTH AGAIN
Seek medical attention immediately if you notice any of the following signs or symptoms.
| Do you experience any of these signs? | What can you possibly suffer from? |
|---|---|
| swelling of a leg or along a vein in the leg or foot, especially if you also get:pain or soreness in the leg that is only felt when you stand or walkincreased heat in the affected legdiscoloration of the skin on the leg, e.g. pale, red or blue | Deep vein thrombosis |
| sudden unexplained shortness of breath or rapid breathingsudden cough for no apparent reason that could possibly cause you to cough up bloodsevere chest pain that may increase with deep breathingsevere instability or dizzinessfast or irregular heartbeatsevere pain in the abdomenIf you are not sure, talk to a doctor because some of these symptoms, e.g. cough and shortness of breath, can be mistakenly interpreted as a mild condition such as a respiratory infection (such as a common cold). | Pulmonary embolism |
| Symptoms that usually occur in one eye:immediate loss of vision orblurred vision without pain that can lead to vision loss | Retinal venous thrombosis(blood clot in the eye) |
| chest pain, discomfort, pressure, heavinesspressure or feeling of fullness in the chest, arm or below the sternumfeeling full, indigestion or feeling of suffocationdiscomfort in the upper body that radiates to the back, jaw, neck, arm and abdomensweating, nausea, vomiting or dizzinessextreme weakness, anxiety or shortness of breathfast or irregular heartbeat | Myocardial infarction |
| sudden weakness or numbness in the face, arms or legs, especially on one side of the bodysudden confusion, difficulty speaking or understandingsudden vision problems in one or both eyessudden difficulty walking, dizziness, loss of balance or coordinationsudden, severe or prolonged headache without a known causeunconsciousness or fainting with or without seizuresSometimes the symptoms of a stroke can be short-lived with almost immediate or complete recovery, but you should still seek medical attention immediately because you are at risk of having a new stroke . | Stroke |
| swelling and slight blue discoloration of an arm or legsevere pain in the abdomen ( acute abdomen) | Blood clots that block other blood vessels |
BLOOD CLOTS IN A FRIEND
What can happen if a blood clot forms in a vein?
- The use of combined hormonal contraceptives has been associated with an increased risk of blood clots in the vein (venous thrombosis ). However, these side effects are rare. They usually occur during the first year of using a combined hormonal contraceptive.
- If a blood clot forms in a vein in the leg or foot, it can lead to deep vein thrombosis (DVT).
- If a blood clot moves from the bone and stays in the lung, it can lead to a pulmonary embolism .
- In very rare cases, a blood clot can form in a vein in another organ such as the eye ( retinal venous thrombosis ).
When is the risk of developing a blood clot in a vein greatest?
The risk of developing a blood clot in a vein is greatest during the first year that you use combined hormonal contraceptives for the first time. The risk can also be higher if you start again with a combined hormonal contraceptive (same product or another product) after a break of 4 weeks or longer.
After the first year, the risk decreases, but it is always slightly higher than if you do not use a combined hormonal contraceptive.
When you stop using Cleosensa, the risk of a blood clot returns to normal within a few weeks.
How big is the risk of developing a blood clot?
The risk depends on your natural risk of VTE and the type of combined hormonal contraceptive you are taking.
The total risk of a blood clot in the leg or lungs with Cleosensa is small.
- Of 10,000 women who do not use a combined hormonal contraceptive and are not pregnant, about 2 develop a blood clot in one year.
- Of 10,000 women who use a combined hormonal contraceptive that contains levonorgestrel or norethisterone or norgestimate, about 5-7 develop a blood clot in a year.
- Of 10,000 women who use a combined hormonal contraceptive that contains drospirenone such as Cleosensa, about 9-12 develop a blood clot in a year.
- The risk of blood clots varies depending on your medical history (see “Factors that may increase the risk of a blood clot” below).
| Risk of developing a blood clot during a year | |
|---|---|
| Women who do not use the combined contraceptive pill / patch / ring and who are not pregnant | About 2 out of 10,000 women |
| Women using a combined hormonal contraceptive containing levonorgestrel, norethisterone or norgestimate | About 5-7 out of 10,000 women |
| Women touching Cleosensa | About 9-12 out of 10,000 women |
Factors that may increase the risk of a blood clot in a vein
The risk of a blood clot with Cleosensa is small but some conditions increase the risk. The risk is higher:
- if you are very overweight (body mass index or BMI over 30 kg / m2)
- if someone in your family has had a blood clot in their bones, lungs or other organ at a young age (eg for about 50 years). In this case, you may have a hereditary blood clotting disease
- if you need to have surgery, or stay in bed for a long period of time due to injury or illness, or if your leg is plastered. The use of Cleosensa may need to be stopped for several weeks before an operation or while you are less mobile. If you have to stop taking Cleosensa, ask your doctor when you can start taking it again
- with increasing age (especially if you are over about 35 years old)
- if you gave birth a few weeks ago
The risk of developing a blood clot increases the more conditions you have.
Air travel (over 4 hours) can temporarily increase the risk of a blood clot, especially if you have any of the other factors listed here.
It is important that you tell your doctor if any of these conditions apply to you, even if you are unsure. Your doctor may decide that you need to stop taking Cleosensa.
If any of the above conditions change when you use Cleosensa, e.g. A close relative suffers from a blood clot with an unknown cause, or you gain a lot of weight, talk to your doctor.
BLOOD CLOTS IN AN ART
What can happen if a blood clot forms in an artery ?
Like a blood clot in a vein, a clot in an artery can lead to serious problems. It can e.g. cause a heart attack or stroke .
Factors that may increase the risk of a blood clot in an artery
It is important to know that the risk of a heart attack or stroke due to the use of Cleosensa is very small but may increase:
- with increasing age (after about 35 years of age)
- if you smoke. When using combined hormonal contraceptives Cleosensa, you should stop smoking. If you can not stop smoking and are over 35 years old, your doctor may advise you to use another type of contraceptive.
- if you are overweight
- if you have high blood pressure
- if a close relative has had a heart attack or stroke at a young age (younger than 50 years). In this case, you may also be at greater risk of a heart attack or stroke .
- if you or a close relative have high blood fats ( cholesterol or triglycerides )
- if you get migraines , especially migraines with an aura
- if you have heart problems (valve disease, a heart rhythm disorder called atrial fibrillation )
- if you have diabetes .
If you have more than one of these conditions or if any of them are particularly serious, the risk of developing a blood clot can be even greater.
If any of the above conditions change when you use Cleosensa, e.g. If you start smoking, a close relative suffers from a thrombosis of unknown cause, or you gain a lot of weight, talk to your doctor.
Cleosensa and cancer
Breast cancer has been observed somewhat more frequently in women using combined oral contraceptives , but it is not known if this is caused by the treatment. For example, it may be that more tumors are detected in women who use combined contraceptive pills because they are more often examined by a doctor. The incidence of breast tumors gradually decreases after stopping treatment with combined hormonal contraceptives. It is important that you examine your breasts regularly and you should contact your doctor if you feel any lump.
In rare cases, benign liver tumors, and, more rarely, malignant liver tumors have been reported in birth control pill users. Contact your doctor if you experience unusually severe abdominal pain.
Bleeding between periods
During the first months of taking Cleosensa, you may experience unexpected bleeding (bleeding outside the midweek). If such bleeding occurs for several months, or if it occurs after several months of use, your doctor must investigate the cause.
What to do if you do not experience any bleeding during the intervening week
If you have taken the tablets as you should, if you have not vomited or had severe diarrhea, and if you have not taken any other medicine, it is very unlikely that you are pregnant.
If the expected bleeding does not occur twice in a row, it is possible that you are pregnant. Contact your doctor immediately. Do not start the next map until you are sure you are not pregnant.
Mental disorders
Some women who use hormonal contraceptives, including Cleosensa, have reported depression or depression. Depression can be severe and can sometimes lead to suicidal thoughts. If you experience mood swings and symptoms of depression, you should contact a doctor as soon as possible for advice.
Other medicines and Cleosensa
| Always tell your doctor which medicines and herbal remedies you are already taking. Also tell any other doctors and dentists who prescribe other medicines (or tell your pharmacist) that you are taking Cleosensa. They can inform you if you need to use other preventative measures (such as condoms), and if so, for how long. |
Some medicines may affect the level of Cleosensa in the blood and make it less effective in preventing pregnancy, or may cause unexpected bleeding. These medicines are as follows:
- drugs for the treatment of
- epilepsy (eg primidone, phenytoin , barbiturate is carbamazepine, oxcarbazepine, felbamate, topiramate)
- drugs against tuberculosis (rifampicin)
- HIV and hepatitis C infections (so-called protease inhibitors and non-nucleoside reverse transcriptase inhibitors such as ritonavir, nevirapine, efavirenz) or other infections (griseofulvin)
- high blood pressure in the blood vessels of the lungs ( bosentan )
- the herbal medicine St. John’s wort
Cleosensa can affect the effect of other drugs e.g.
- medicines containing ciclosporin
- the drug lamotrigine for epilepsy (this may lead to seizures more often)
Do not use Cleosensa if you have hepatitis C and are taking medicines containing ombitasvir / paritaprevir / ritonavir and dasabuvir as it may lead to elevated liver function levels in the blood (an increase in the liver enzyme ALT ). Your doctor / midwife will prescribe another type of contraceptive before you start treatment with these medicines.
Treatment with Cleosensa can be resumed approximately 2 weeks after stopping treatment with ombitasvir / paritaprevir / ritonavir and dasabuvir. See section “Do not use Cleosensa”.
Consult your doctor or pharmacist before taking any medicine.
Cleosensa with food and drink
Cleosensa can be taken with or without food, if necessary with a small amount of fluid
Laboratory test
If you need to take a blood test, tell your doctor or laboratory staff that you are taking birth control pills , as hormonal contraceptives can affect the results of certain tests.
Pregnancy and breastfeeding
Pregnancy
Do not take Cleosensa if you are pregnant. If you become pregnant during treatment with Cleosensa, stop treatment immediately and contact your doctor. If you become pregnant, you can stop taking Cleosensa at any time (see also “If you stop taking Cleosensa”).
Breast-feeding
The general recommendation is that Cleosensa should not be used during breast-feeding. If you are breast-feeding and want to use birth control pills, contact your doctor.
If you are pregnant or breast-feeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
There is no information to suggest that the use of Cleosensa affects the ability to drive or use machines.
Cleosensa contains lactose
If your doctor has told you that you are hypersensitive to certain sugars, you should consult your doctor before taking this medicine.
3. How to use Cleosensa
Use for children and adolescents
Always take this medicine exactly as your doctor has told you. Ask your doctor or pharmacist if you are unsure.
Take a tablet of Cleosensa every day, if necessary with a small amount of liquid. You can take the tablets with or without food, but they should be taken at about the same time each day.
The map contains 21 tablets. Next to each tablet is the day of the week when it should be taken. If you start on a Wednesday, take the tablet marked “ONS”. Follow the direction of the arrow on the map until you have taken all 21 tablets.
Then take a break for seven days. During this tablet-free period of seven days (also called the intervening week), bleeding should occur. This is a so-called dropout bleeding and it usually starts 2 or 3 days into the middle week.
On day 8 after the last Cleosensa tablet (ie after the seven-week interval), start with the next map, regardless of whether the bleeding has stopped or not. This means that you should start each map on the same day of the week and that the dropout bleeding should occur on the same day each month.
If you use Cleosensa in this way, you are protected against pregnancy even during the 7 days when you do not take any tablet.
When should you start with the first map?
If you have not used a contraceptive containing hormones during the previous month
Start with Cleosensa on the first day of the cycle (ie the first day of menstruation). If you start using Cleosensa on the first day of your period, you have immediate protection against unwanted pregnancy. You can also start on days 2–5 in your cycle, but then you must use an extra method of contraception (eg condoms) for the first seven days.
When changing from a combined contraceptive pill or vaginal ring or contraceptive patch
It is recommended that you start taking Cleosensa the day after you take the last active tablet (the last tablet of active substances) of the previous pill (or at the latest on the day after the usual tablet break). When changing from a combined contraceptive in the form of a vaginal ring or contraceptive patch , follow the doctor’s recommendations.
When switching from a progestagen-only contraceptive ( birth control pills, injectable or implanted intrauterine contraceptive to progestagen)
You can change at any time from the contraceptive pill with progestagen (from an implanted contraceptive or an intrauterine contraceptive on the day it was removed, from an injectable contraceptive from the day the next injection was to take place) but in all these cases extra precautions should be used (t (eg condoms) during the first seven days of taking the tablets.
After miscarriage
Follow your doctor’s instructions.
After having children
You can start with Cleosensa between 21 and 28 days after having a baby. If you start after day 28, you must use a barrier method (such as a condom) for the first seven days of using Cleosensa.
If you have had sex before using Cleosensa (again) after having a baby, make sure you are not pregnant, or wait until your next period.
If you are breast-feeding and want to start using Cleosensa (again) after having a baby
Read the section on “Breastfeeding”.
Ask your doctor if you are unsure when to start taking the tablets.
There are no reports of serious consequences after taking too many Cleosensa tablets.
If you take several tablets at the same time, you may experience nausea or vomiting. Young women may experience vaginal bleeding.
If you forget to use Cleosensa
- If it is less than 12 hours since you should have taken the tablet, the protection against pregnancy is not reduced. Take the tablet you forgot as soon as you can, and then take the following tablets at the usual time.
- If you are more than 12 hours late in taking a tablet, the protection against pregnancy may be reduced. The more tablets you forget to take, the greater the risk of getting an unwanted pregnancy.
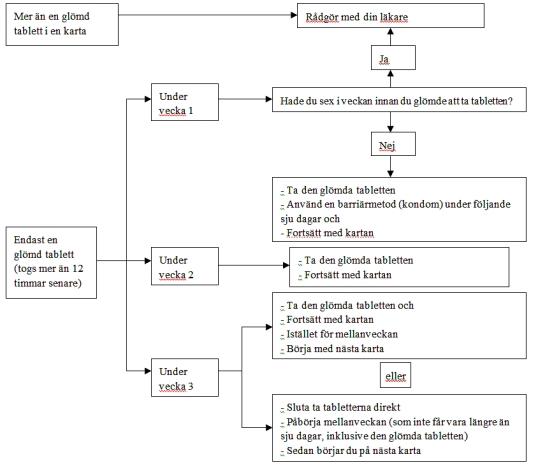
The risk of insufficient protection is greatest if you forget to take the tablet at the beginning or end of the map. You should therefore follow these rules (see diagram below):
More than a forgotten tablet on the map
Contact your doctor.
A forgotten tablet during week 1
Take the forgotten tablet as soon as you discover that you have forgotten, even if it means that you have to take two tablets at the same time. Continue to take the tablets at the usual time and use extra protection for the next seven days, such as a condom. If you had sex the week before you forgot the tablet, you may be pregnant. If this is the case, contact your doctor.
A forgotten tablet during week 2
Take the forgotten tablet as soon as you discover that you have forgotten, even if it means that you have to take two tablets at the same time. Continue to take the tablets at the usual time. The protection against pregnancy is not reduced and you therefore do not need to use any other contraceptives.
A forgotten tablet during week 3
You can choose between two options:
- Take the forgotten tablet as soon as you discover that you have forgotten, even if it means that you have to take two tablets at the same time. Continue to take the tablets at the usual time. Start right on the next map instead of taking a break.You will probably have your period at the end of the second map, but you may also experience menstrual-like bleeding when you take the second map.
- You can also stop taking tablets from the current map and immediately take a tablet break of seven days (note which day you forgot to take the tablet). If you want to start on a new map on the same day as you always start on, you can make the tablet break shorter than seven days.
If you follow one of these two recommendations, you are protected against pregnancy.
If you have forgotten to take any tablet on the map and you do not experience any bleeding during the first tablet break, you may be pregnant. Contact your doctor before starting on the next map.
If you experience vomiting or severe diarrhea
If you vomit within 3-4 hours after taking your tablet or if you develop severe diarrhea, it may mean that the active substances in the tablet are not completely absorbed into your body. This is almost the same situation as when you forgot to take a tablet. After vomiting or having diarrhea, take another tablet from the backup card as soon as possible. If possible, take it within 12 hours from the time you usually take your tablet. If this is not possible or if more than 12 hours have passed, follow the instructions under “If you forget to take Cleosensa”.
Postponing menstruation: what you need to know
Although not recommended, it is possible to postpone menstruation by starting directly on a new map with Cleosensa and completing it instead of making a tablet-free map. You may experience minor or menstrual-like bleeding while taking tablets from the other card. After the normal tablet-free stay of seven days , start on the next map.
You can ask your doctor for advice before you decide to postpone your period.
Change the first day of menstruation: what you need to know
If you take the tablets according to the instructions, menstruation will occur during the tablet-free week. If you need to change this day, the number of days without tablets should be reduced ( but never increased – the break should not exceed seven days!) . For example, if your tablet break usually starts on a Friday and you want to change it to a Tuesday (three days earlier), you can start a new map three days earlier than usual. If the tablet-free period is very short (for example, three days or less), you may not experience any bleeding during this time. You may then experience minor or menstrual-like bleeding.
If you are not sure, talk to your doctor.
If you stop using Cleosensa
You can stop taking Cleosensa whenever you want. If you do not want to get pregnant, consult your doctor about other reliable contraceptive methods that you can use. If you want to get pregnant, stop using Cleosensa and wait until you get your period before trying to conceive. It will then be easier to calculate the expected date of birth.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. If you get any side effects , especially if they are serious or persistent, or if your health changes and you think it may be due to Cleosensa, talk to the doctor.
An increased risk of blood clots in the veins (venous thromboembolism , VTE), or blood clots in the arteries are (arterial thrombosis, ATE) are all women taking hormonal contraceptives combined. For more information on the different risks of using combined hormonal contraceptives, see section 2 “What you need to know before using Cleosensa”.
The following side effects have been linked to the use of Cleosensa.
Common (may affect up to 1 in 10 people):
- menstrual disorders, menstrual bleeding, chest pain, sore breasts
- headache, depression
- migraine
- nausea
- thick, whitish discharge from the vagina and vaginal fungal infection.
Uncommon (may affect up to 1 in 100 people):
- enlarged mammary glands, altered sex drive
- high blood pressure , low blood pressure
- vomiting, diarrhea
- acne , rash, severe itching , hair loss ( alopecia )
- vaginal infection
- fluid retention and changes in body weight.
Rare (may affect up to 1 in 1,000 people):
- allergic reactions (hypersensitivity), asthma
- exuding breasts
- impaired hearing
- the skin diseases erythema nodosum (characterized by painful red nodules in the skin) or erythema multiforme (characterized by rash with annular redness or sores).
- dangerous blood clots in a vein or artery , for example: in a leg or foot (ie DVT); in the lungs; myocardial infarction; stroke; mini- stroke or transient stroke-like symptoms, called transient ischemic attack ( TIA ); blood clots in the liver, stomach / intestines, kidneys or eyes.
The risk of developing a blood clot may be higher if you have other conditions that increase this risk (see section 2 for more information on the conditions that increase the risk of blood clots and the symptoms of blood clots).
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist, or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly to the Medical Products Agency, www.lakemedelsverket.se. By reporting side effects, you can help increase drug safety information.
5. How to store Cleosensa
Keep this medicine out of the sight and reach of children.
No special storage instructions.
Do not use this medicine after the expiry date which is stated on the carton after EXP. The expiration date is the last day of the specified month.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist how to dispose of medicines no longer required. These measures will help to protect the environment.
6. Contents of the packaging and other information
Content declaration
- The active substances are ethinyl estradiol 0.03 mg and drospirenone 3 mg.
- Other ingredients are:
- Tablet core: lactose monohydrate , maize starch, pregelatinised starch (maize), crospovidone, povidone K-30 (E1201), polysorbate 80, magnesium stearate (E572).
- Coating: Partially hydrolyzed polyvinyl alcohol, titanium dioxide (E171), macrogol 3350, talc (E553b), yellow iron oxide (E172).
What the medicine looks like and the contents of the pack
Yellow, round film-coated tablets.
Cleosensa is available in packs of 1, 2, 3, 6 and 13 blister cards, each containing 21 tablets.
The blister packs may also have a holder in the pack.
Not all pack sizes may be marketed.
Marketing Authorisation Holder
Actavis Group PTC ehf.
Reykjavikurvegur 76-78
220 Hafnarfjordur
Iceland
Manufacturer
Laboratories León Farma, SA
C / La Vallina s / n, Pol. Ind. Navatejera,
24008 Villaquilambre, Leon
Spain
Local representative