 |
ADJUSTING TO CHRONIC ILLNESSES:Shock, Encounter, Retreat |
| << DEALING WITH PAIN:Acute Clinical Pain, Chronic Clinical Pain |
| THE COPING PROCESS IN PATIENTS OF CHRONIC ILLNESS:Asthma >> |

Health
Psychology PSY408
VU
Lesson
27
ADJUSTING
TO CHRONIC ILLNESSES
"It's
not fair" 12-year-old Joe
complained. Why can't I eat the
stuff I like? Other kids
can. Why do I have to
check
my blood everyday and take
shots? Nobody else has to do
that," He voiced these complaints as
he
left
the emergency room after suffering severe
stomach cramps because he
was not adhering to his
medical
regimen.
Hospital tests recently determined
that Joe has diabetes,
and he was not adjusting
well to the
regimen
his physician instructed him to
follow.
His
parents tried to explain
that not following the
regimen could have serious health
consequences, but he
thought,
`I'll do some of the things they say I
should do, and that'll be
enough. I feel fine--so
those
problems
won't happen to me." When
his noncompliance led to his being rushed
to the hospital with
severe
abdominal pain and difficulty breathing, he
finally believed the warnings he
received, and he began
to
adhere
closely to his
regimen.
Different
individuals react differently to
developing a chronic illness. Their
reactions depend on
many
factors,
such as their coping skills
and personalities, the social
support they have, the nature
and
consequences
of their illnesses, and the
impact of the illnesses on their daily
functioning. At the very least,
having
a chronic condition entails frequent
impositions on the patients and their
families. Chronically ill
people
may suffer periodic episodes of feeling
poorly and need to have
regular medical checkups,
restrict
their
diets or other aspects of
their life styles, or
administer daily treatment, for instance.
Many chronic
conditions
entail more than just
impositions-- they produce frequent pain
or lead to disability or
even
death.
This
and the next coming lectures
focus mainly on tertiary prevention
for chronic illness-- to retard
its
progression,
prevent disability, and rehabilitate the
person, physically and psychologically.
We will examine
how
people react to and cope
with chronic health problems and what
can be done to help these
people
cope
effectively.
The
present lecture concentrates on health
problems that are less
likely to result in death
but often lead to
disability.
We will begin by discussing people's
reactions to having a chronic condition,
then we will
examine
the experiences and needs of
individuals living with
various health problems, and
then we will
consider
psychosocial interventions to enhance
patients' long-term adaptation to their
conditions.
Our
discussion in these lectures
will address many questions
that are of great concern to
patients, to their
families
and friends, and probably to you.
How do individuals react after
their initial shock of learning
that
they
have a chronic illness? What kinds of
health problems usually involve the
most difficult
adjustments
for
people? How do patients' chronic
conditions impact on their
families? What can families,
friends, and
therapists
do to help chronically ill people adapt
effectively to their conditions?
Adjusting
To a Chronic Illness
I
felt like I'd been
hit in the stomach by a sledgehammer--this is
how many patients describe
their first
reaction
upon learning that they have a disabling
or life-threatening illness. Questions
without immediate
answers
flash through their minds:
Is the diagnosis right and, if
so, what can we do about it?
Will I be
disabled,
disfigured, or in pain? Will I die?
How soon will these
consequences happen? What
will happen to
my
family? Do I have adequate
medical and life insurance?
Learning of a chronic health problem
usually
comes
as a great shock, and this is
often the first reaction individuals
experience when the physician
tells
them
the diagnosis.
120
Health
Psychology PSY408
VU
Initial
Reactions on Having a Chronic
Condition
By
observing patients in rehabilitation and
health settings, Franklin Shontz
(1975) has described a
sequence
of
reactions people tend to exhibit
following the diagnosis of a serious
illness. This sequence of
reactions is:
1.
Shock--an
emergency response, marked by
three characteristics: {a) being
stunned or bewildered, (b)
behaving
in an automatic fashion, and (c) feeling
detached from the situation, that
is, feeling like being an
observer
rather than a participant in the events
that occur. The shock
may last only a short while
or may
continue
for weeks, occurs to some
degree in any crisis situation people
experience, and it is likely to
be
most
pronounced when the crisis comes without
warning.
2.
Encounter--a
phase that is marked by
disorganized thinking and
feelings of loss, grief,
helplessness,
despair,
and being overwhelmed by reality.
3.
Retreat--a
phase in which people tends to
use avoidance strategies,
such as denying either the
existence
of
the health problem or its implications.
But then reality begins to
intrude: the symptoms remain or
get
worse,
additional diagnoses confirm the
original one, and it becomes
clear that adjustments need
to be
made.
Using retreat as a "base of operation,"
patients tend to contact reality a
little at a time until they
reach
some
form of adjustment to the health problem
and its implications.
Do
all individuals react in the
ways Shontz has described
when they are faced with
such crises as being
diagnosed
with a serious illness? No,
but probably most do.
For instance, when faced
with a crisis, most
people
react with shock initially,
but other individuals may be
"cool and collected, while
others may be
"paralyzed"
with anxiety or may become hysterical".
Similarly, although many people with
serious illnesses
feel
extremely helpless and overwhelmed after
the initial shock, others do
dot. And many patients do
not
rely
heavily on avoidance strategies to cope
with the stress caused by having a health
problem.
People
who use denial and other
avoidance strategies do so to control
their emotional responses to
a
stressor,
especially when they believe they can do
nothing to change the situation. But the
usefulness of this
approach
has limits. Although using
avoidance strategies often provides
psychological benefits early in
the
process
of coping with health problems, excessive
avoidance can soon become
maladaptive to patients'
physical
and psychological well-being.
For
example, when hospitalized people receive
information about their
conditions and future risk
factors,
those
individuals who use
avoidance strategies heavily,
gain less information about
their conditions than
those
who use these strategies to
a lesser degree. Patients
often need to make major
decisions about their
immediate
treatment. How can they make
these decisions rationally if they
fail to take in the
information
that
the practitioners present to them? Later,
they may need to take action to
promote their recovery,
reduce
the likelihood of future health problems,
and adjust their lifestyles,
social relationships, and
means of
employment.
What factors influence how people
cope with their health
problems? The next
section
provides
some answers to this
question.
Influences
on Coping with Health
Crisis
Healthy
people tend to take their health
for granted. They expect to be
able to carry out their
daily activities
and
social roles from one
day to the next without
substantial disruptions due to illness.
When a serious
illness
or injury occurs, their
everyday life activities are disrupted.
Regardless of whether the condition
is
temporary
or chronic, the first phases in coping
with it are similar. But
there is an important difference:
in
contrast
to the short-term disruptions that temporary illnesses
cause, chronic health problems
usually
require
that patients and their
families make permanent behavioral,
social, and emotional
adjustments.
When
people learn that they have a
serious chronic illness, the diagnosis
quickly changes the way they
view
themselves
and their lives. The
plans they had for tomorrow
and for the next days,
weeks, and year may
be
121
Health
Psychology PSY408
VU
affected.
Major plans and minor
ones may change: Did they
plan to go on a trip this weekend? They
may
change
their minds now. Did they
plan to complete a college
education, or enter a specific
career field, or
get
married and have children, or
move to a new community when they
retire? Some of these ideas
for the
future
may evaporate after the
diagnosis.
As
psychologists Richard Lazarus
and Cohen have noted,
because the idea of being healthy, able,
and
having
a normal physique is central to most
people's image and evaluation,
becoming ill can be a shock
to a
persons
sense of security and to his
or her self-image. Not only
does it threaten the customary view
of
oneself,
but it further underscores
that one is indeed vulnerable;
and that one's life
may be changed in major
respects.
As a result adjustment to an illness or
injury which is life-threatening or
potentially disabling may
require
considerable coping effort. Potentially
disabling or life-threatening conditions
leave patients and
their
families with many
uncertainties, Often no one
can tell for certain
exactly what the course of the
illness
will
be.
The
Crisis Theory
Why
do some individuals cope
differently from others after learning
they have a chronic health
problem?
Rudolf
Moos (1986) has proposed the
crisis theory, which
describes factors that influence
how people
adjust
during a crisis, such as having an
illness.
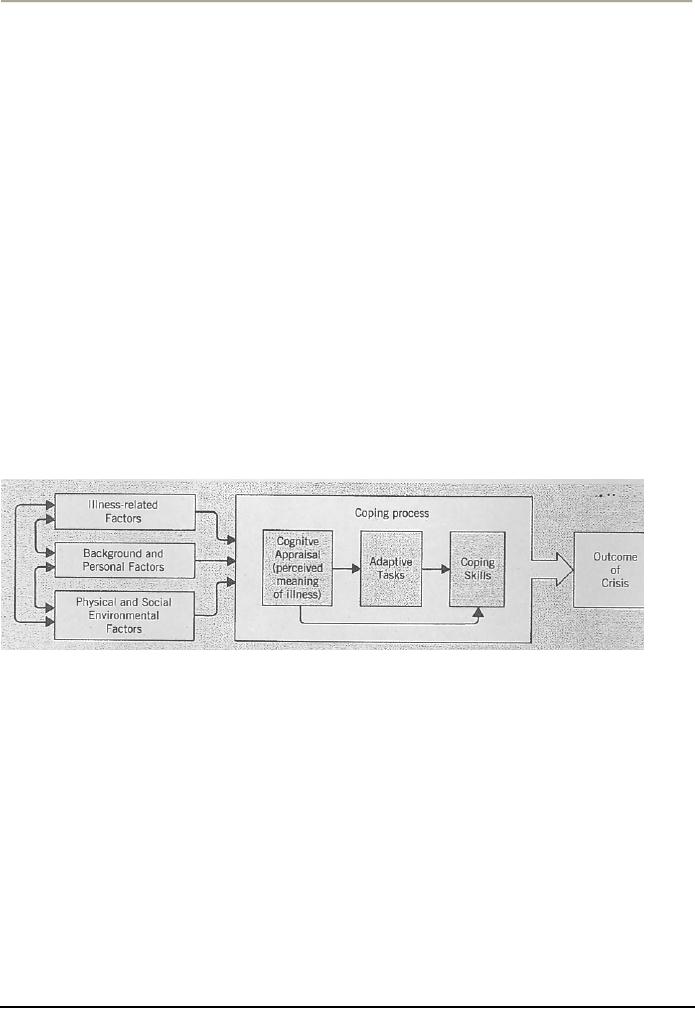
The
diagram presents his
conceptual model, showing that the
outcome of the crisis-- or the adjustment
the
person
makes--depends on the coping process,
which depends on three
contributing influences:
illness-
related
factors, background and personal
factors, and physical and
social environmental factors. We
will
look
at these contributing influences,
and then see how they affect the coping
process the patient
uses.
a)
Illness-Related Factors
Some
health problems present a greater threat
to the person than others
do--they may be more
disabling,
disfiguring,
painful, or life-threatening, for
example. As you might
expect, the greater the threats
patients
perceive
for any of these factors,
the more difficulty they are
likely to have coping with
their conditions.
Adjusting
to being disfigured can be extremely
difficult, particularly when it involves the
person's face.
Many
individuals whose faces are
badly scarred withdraw from
social encounters, sometimes
completely.
Often
people who see the disfigurement react
awkwardly, and some show
feelings of revulsion. Even
children
react more negatively to people's
facial disfigurements than to injuries to
other parts of the
body,
such
as when people are crippled or
missing a limb.
Patients
also have difficulty coping
with illness- related
factors that involve annoying or
embarrassing
changes
in bodily functioning or that
draw attention to their conditions.
People with some illnesses,
for
instance,
may need artificial devices
for excreting fecal or
urinary wastes. These
devices may be
noticeable
either
visibly or by their odors,
and many patients have
exaggerated impressions of the social
impact such
devices
have.
122

Health
Psychology PSY408
VU
Other
chronically ill people must treat their
conditions with ointments that
may have odors or
equipment
that
is visible or makes noise. Still
others may experience
periodic seizures or muscle
spasms that can be
embarrassing.
Many people with chronic illnesses feel
self-conscious about their health
problems--or even
stigmatized
by them--and want to hide them from
others.
Various
other aspects of treatment regimens
can make adjustment very
difficult, too. Some
treatments are
painful
or involve medications that produce
serious side effects--either by
leading to additional health
problems
or by interfering with the patient's
daily functioning, such as by making the
person immobile or
drowsy.
Other regimens may have
treatment schedules and time commitments
that make it difficult for
the
person
to find or hold a job. Some
regimens require patients and
their families to make
substantial changes
in
their lifestyles, which they
might resent and fail to
carry out. Each of these
factors can impair
people's
adjustment
to chronic health problems.
b)
Background and Personal
Factors
People
who cope well with chronic
health problems have the psychological
and behavioral resources to
resolve
the chronicity or `long-termness' of the situation,
balance hope against despair
and find purpose
and
quality
in life. Often, these people
have hardy or resilient personalities
that allow them to see a good
side in
difficult
situations.
People
with chronic diseases who
are resilient can often find
purpose and quality in their
lives, maintain
their
self-esteem, and resist feeling
helpless and
hopeless.
The
ways individuals cope with
chronic health problems also depend on
many other background
and
personal
factors, such as their age,
gender, social class, philosophical or
religious commitments, emotional
maturity
and self-esteem.
With
respect to gender differences,
for instance, men are
more likely than women to be
"threatened by the
decreases
in ambition, vigor, and
physical prowess that often
result from serious illness
because, by
comparison
with women, they are
confident in the stability of their
physical abilities and bodily
functioning.
Having
a chronic illness often means
that the individual must
take on a dependent and
passive role for a
long
period of time. For men, this
can be especially difficult
since it is inconsistent with the
assertive and
independent
roles they generally occupy in
most societies of the
world.
The
timing of a health problem in the
person's life span also
affects the impact on him or
her. In the case of
very
young children, their limited cognitive
abilities prevent them from understanding fully the
nature of
their
illnesses, the treatment regimens they
must follow, and the
long-term implications of their
conditions.
Their
concerns are likely to focus
on any restrictions that are
imposed on their lifestyles
and activities, the
frightening
medical procedures they experience,
and possible separations
from their parents. As
children get
older
and their comprehension improves they
may be able to participate in making some
decisions about
their
treatment.
c)
Physical and Social Environmental
Factors
Many
physical and social features
of our environments can affect the way we
adjust to chronic health
problems.
The physical aspects of a hospital
environment for instance,
are usually very dull and
confining
for
patients, thereby depressing their
general morale and mood.
For some individuals, the
home
environment
may not be much better.
Many patients have
difficulty getting around their houses
or
performing
self-help tasks; such as buttoning
clothes or opening food
containers, and lack
special
equipment
or tools that can help them
do these tasks and be more
self-sufficient. These people's
adjustment
to
their health problems can be impaired as
long as these situations
persist.
The
patient's social environment functions as
a system, with the behavior of
each person affecting the
others.
The presence of social support,
for example, generally helps
patients and their families
and friends
123

Health
Psychology PSY408
VU
cope
with their illnesses.
Individuals who live alone
and have few friends or who
have poor relationships
with
the people they live with tend to
adjust poorly to chronic health conditions.
But it is also true
that
sometimes
people in a patient's social network may
undermine effective coping by providing bad
examples
or
poor advice. The degree to
which each member of the
social system adjusts in constructive
ways to the
illness
affects the adjustment of the
others.
The
primary source of social support for
children and most adults
who are ill typically
comes from their
immediate
families. People in old age
whose spouses are either
deceased or unable to help
are likely to
receive
support mainly from their children, but
also from siblings, friends,
and neighbors. At almost
any
age,
patients may join support
groups for people with
specific medical problems.
These groups can
provide
informational
and emotional support.
As
the above given diagram depicts,
crisis theory's three contributing
influences are interrelated and
can
modify
each other. The patient's
social class or cultural background, for
instance, may affect his or
her self-
consciousness
about or access to special
devices and equipment to promote
self-sufficiency. These
contributing
factors combine to influence the coping process the
person uses to deal with the
crisis.
We
will talk about the coping process in
adjusting to chronic illnesses in our
next lecture. We will also
talk
about
the different chronic illnesses and
their biopsychosocial impacts on
patients.
124
Table of Contents:
- INTRODUCTION TO HEALTH PSYCHOLOGY:Health and Wellness Defined
- INTRODUCTION TO HEALTH PSYCHOLOGY:Early Cultures, The Middle Ages
- INTRODUCTION TO HEALTH PSYCHOLOGY:Psychosomatic Medicine
- INTRODUCTION TO HEALTH PSYCHOLOGY:The Background to Biomedical Model
- INTRODUCTION TO HEALTH PSYCHOLOGY:THE LIFE-SPAN PERSPECTIVE
- HEALTH RELATED CAREERS:Nurses and Physician Assistants, Physical Therapists
- THE FUNCTION OF NERVOUS SYSTEM:Prologue, The Central Nervous System
- THE FUNCTION OF NERVOUS SYSTEM AND ENDOCRINE GLANDS:Other Glands
- DIGESTIVE AND RENAL SYSTEMS:THE DIGESTIVE SYSTEM, Digesting Food
- THE RESPIRATORY SYSTEM:The Heart and Blood Vessels, Blood Pressure
- BLOOD COMPOSITION:Formed Elements, Plasma, THE IMMUNE SYSTEM
- SOLDIERS OF THE IMMUNE SYSTEM:Less-Than-Optimal Defenses
- THE PHENOMENON OF STRESS:Experiencing Stress in our Lives, Primary Appraisal
- FACTORS THAT LEAD TO STRESSFUL APPRAISALS:Dimensions of Stress
- PSYCHOSOCIAL ASPECTS OF STRESS:Cognition and Stress, Emotions and Stress
- SOURCES OF STRESS:Sources in the Family, An Addition to the Family
- MEASURING STRESS:Environmental Stress, Physiological Arousal
- PSYCHOSOCIAL FACTORS THAT CAN MODIFY THE IMPACT OF STRESS ON HEALTH
- HOW STRESS AFFECTS HEALTH:Stress, Behavior and Illness, Psychoneuroimmunology
- COPING WITH STRESS:Prologue, Functions of Coping, Distancing
- REDUCING THE POTENTIAL FOR STRESS:Enhancing Social Support
- STRESS MANAGEMENT:Medication, Behavioral and Cognitive Methods
- THE PHENOMENON OF PAIN ITS NATURE AND TYPES:Perceiving Pain
- THE PHYSIOLOGY OF PAIN PERCEPTION:Phantom Limb Pain, Learning and Pain
- ASSESSING PAIN:Self-Report Methods, Behavioral Assessment Approaches
- DEALING WITH PAIN:Acute Clinical Pain, Chronic Clinical Pain
- ADJUSTING TO CHRONIC ILLNESSES:Shock, Encounter, Retreat
- THE COPING PROCESS IN PATIENTS OF CHRONIC ILLNESS:Asthma
- IMPACT OF DIFFERENT CHRONIC CONDITIONS:Psychosocial Factors in Epilepsy