 |
Health
Psychology PSY408
VU
Lecture
12
SOLDIERS
OF THE IMMUNE SYSTEM
White
blood cells play a key role
in the immune system--they serve as soldiers in
our counterattack
against
invading
substances in the body. There are
two types of white blood
cells. Lymphocytes, as we have
seen,
are
one type; phagocytes are the
other.
Phagocytes
are scavengers that patrol
the body and engulf and
ingest antigens. They are
not choosy. They
will
eat anything suspicious that
they find in the blood stream,
tissues, or lymphatic system. In the
lungs, for
instance,
they consume particles of dust
and other pollutants that
enter with each breath. They
can cleanse
lungs
that have been blackened
with the contaminants of cigarette
smoke, provided the smoking stops.
Too
much
cigarette smoking, over too
long a time, destroys phagocytes
faster than they can be
replenished.
There
are two types of phagocytes:
Macrophages
become
attached to tissues and
remain there, and
Monocytes
circulate
in the blood. The fact that
phagocytes "are not choosy"
means that they are
involved
in
nonspecific immunity--they respond to any
kind of antigen.
Lymphocytes
react in a more discriminating way, being
tailored for attacks against
specific antigens.
The
53

Health
Psychology PSY408
VU
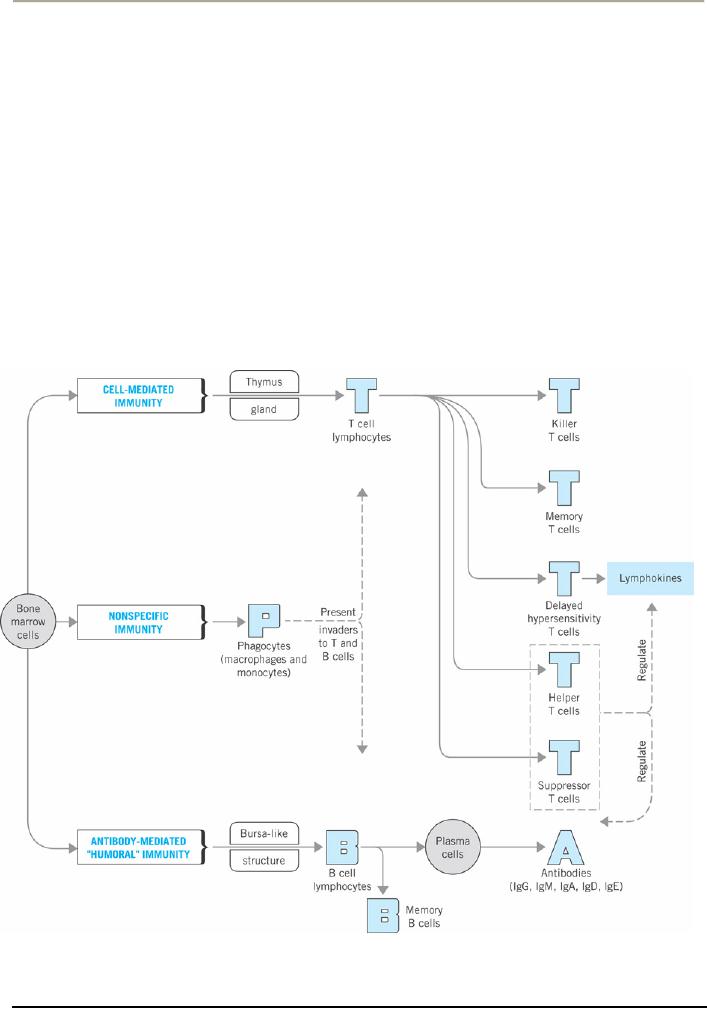
diagram
shows that, in addition to the process of
nonspecific immunity, there are
two types of specific
immune
processes: cell-mediated immunity
and antibody-mediated "humoral" immunity.
Let's examine
these
two specific immune processes
and how they interrelate.
Cell-mediated
immunity operates at the level of the
cell. The soldiers in this
process are lymphocytes
called
T
cell--the name of these
white blood cells reflects
their having matured in the thymus. T
cells are divided
into
several groups, each with
its own important
function:
�
Killer
T cells (also called (CD8
cells) directly attack and
destroy three main targets:
transplanted
tissue
that is recognized as foreign,
cancerous cells, and cells
of the body that have
already been
invaded
by antigens, such as
viruses.
�
Memory
T cells "remember" previous invaders. At
the time of an initial infection, such as
with
mumps,
some T cells are imprinted
with information for
recognizing that specific
kind of
invader--the
virus that causes mumps--in the
future. Memory T cells and
their offspring
circulate
in
the blood or lymph for long
periods of time--sometimes for
decades--and enable the body
to
defend
against subsequent invasions
more quickly.
�
Delayed-hypersensitivity
T cells have two functions. They
are involved in delayed
immune
reactions,
particularly in allergies such as of poison
ivy, in which tissue becomes inflamed.
They also
produce
protein substances called lymphokines
that stimulate other T cells
to grow, reproduce,
and
attack
an invader.
�
Helper
T cells (also called CD4
cells) receive reports of
invasions from other white
blood cells that
patrol
the body, rush to the spleen
and lymph nodes, and
stimulate lymphocytes to reproduce
and
attack.
The lymphocytes they stimulate
are from both the
cell-mediated and the
antibody-mediated
immunity
(also called "humoral"
immunity) processes.
�
Suppressor
T cells operate in slowing down or
stopping cell-mediated and
antibody-mediated
immunity
processes as an infection diminishes or
is conquered. Suppressor and helper T
cells serve
to
regulate cell-mediated and
antibody-mediated immune processes.
What
is antibody-mediated immunity, and how is
it different from the cell-mediated
process? Antibody-
mediated
immunity attacks bacteria,
fungi, protozoa, and viruses
while they are still in body
fluids and
before
they have invaded body cells.
Unlike the cell- mediated
process of attacking infected cells of
the
body,
the antibody-mediated approach focuses on the
antigens directly. The
soldiers in this approach
are
lymphocytes
called B cells. The diagram
shows that B cells give rise
to plasma cells that produce
antibodies.
This
process is often induced by helper T
cells or inhibited by suppressor T
cells.
How
are antibodies involved? Antibodies
are protein molecules called
immunoglobulins ("Ig") that
attach
to
the surface of invaders and
accomplish three results. First, they
slow down the invader, making it
an
easier
and more attractive target
for phagocytes to destroy.
Second, they recruit other protein
substances
that
puncture the membrane of an invading
microorganism, causing it to burst.
Third, they find new
invaders
and form memory B cells
that operate in the future
like memory T cells. As you
can see, antibodies
are
like sophisticated weapons in immune
system wars. Researchers
have identified five classes
of
antibodies--IgG,
IgM, IgA, IgD, and
IgE--each with its own
special function and
"territory" in the body.
For
example, IgA guards the entrances of the
body in fluids, such as
saliva, tears, and
secretions of the
respiratory
tract.
DEFENDING
THE BODY WITH AN IMMUNE
RESPONSE
Now
that we have seen the
soldiers and weaponry of the immune
system, let's see how all of
this is
orchestrated
in defending your body. Protection
from disease actually involves a
series of defenses. We
will
start
at the beginning, as the invader tries to enter the
body.
54

Health
Psychology PSY408
VU
Your
body's first line of defense is the skin
and the mucous membranes
that line the respiratory
and
digestive
tracts. The skin serves as a barrier to
entry, and mucous membranes
are coated with fluids
that
contain
antibodies and other antimicrobial
substances. Even though
these defenses are highly
effective,
large
numbers of antigens get
through, either by eluding the antibodies or by entering a
wound in the skin
or
the mucous membrane.
Once
an antigen penetrates this barrier, it
encounters the second line of
defense, which includes
nonspecific
and
specific immune processes. Phagocytes in
your blood and tissues
attack and consume
invading
substances
of all types.
They
also have another important
function: They present the antigen to B
cells and helper T cells, as if
to
say,
"Here's the enemy, Go get
`em!" The B cells respond to
this message and to stimulation
from helper T
cells
by giving rise to plasma
cells that produce the needed antibodies.
The role of the phagocytes
is
especially
important if the antigen is new
and the body has no memory B
cells for this
substance.
Antibodies
in body fluids attach to
microorganisms, thereby aiding the phagocytes
and other protein
substances
that can kill the
invaders.
Antigens
that manage to get through
and invade body cells encounter the
third line of defense in
which
killer
T cells destroy the invaded cells.
Phagocytes often initiate this
process by presenting antigens to
T
cells,
as we have seen. Once again,
this is especially important if the
antigen is new to the
cell-mediated
system
and the body has no memory T
cells for the substance. As the invasion
subsides, suppressor T
cells
slow
down the cell-mediated and
antibody-mediated immune responses.
Memory B and T cells are
left in
the
blood and lymph, ready to
initiate the immune response if the
same antigen invades the body
again.
Less-Than-Optimal
Defenses
If
our immune systems always
functioned optimally, we would
become sick much less
often. Why and in
what
ways do our defenses
function less than
optimally?
The
effectiveness of the immune system
changes over the life span,
becoming increasingly effective
throughout
childhood and declining in old
age. Newborns come into the
world with relatively little
immune
defense.
They have only one type of
antibody (IgG), for example,
which they receive prior to
birth from
their
mothers through the placenta (the
filter-like organ that
permits the exchange of nutrients and
certain
other
substances between the bloodstreams of
the mother and baby).
Infants who are nursed
receive
antibodies,
particularly IgA, in their mothers'
milk.
In
early infancy, children in technological
societies generally begin a regular
schedule of immunization
through
the use of vaccines. Most
vaccines contain dead or disabled
disease microorganisms that
get the
body
to initiate an immune response and
produce memory lymphocytes
but do not produce the
full-blown
disease.
The efficiency and complexity of the
immune system develop very rapidly in
childhood. As a result,
the
incidence of illness serious
enough to keep children home
from school declines with
age.
Throughout
adolescence and much of
adulthood, the immune system generally
functions at a high level.
Then,
as people approach old age, the
effectiveness of the system tends to
decline. Although the
overall
numbers
of T cells, B cells, and antibodies
circulating in the blood do not decrease
their potency diminishes
in
old age. Compared with the T
cells and B cells of younger
adults, those of elderly people respond
weakly
to
antigens and are less
likely to generate the needed supply of
lymphocytes and antibodies to fight
an
invasion.
Unhealthful
lifestyles, such as smoking
cigarettes and being sedentary,
have been associated with
impaired
immune
function. Poor nutrition can
also lead to less-
than-optimal immune function. Diets
deficient in
vitamins
seem to diminish the production of
lymphocytes and antibodies, for
example.
When
your immune system functions
optimally, it attacks foreign
matter and protects the
body. Sometimes
this
process goes awry, and the immune
response is directed at parts of the
body it was designed to
protect.
55

Health
Psychology PSY408
VU
Several
disorders result from this
condition--they are called autoimmune
diseases. One of these diseases
is
rheumatoid
arthritis, in which the immune response
is directed against tissues
and bones at the joints.
This
causes
swelling and pain and
can leave the bones pitted.
In rheumatic fever, the muscles of the
heart are the
target.
This disease can damage the
heart valves permanently. Multiple
sclerosis, a disease we
considered
earlier,
results when the immune system
attacks the myelin sheath of
neurons.
Many
people believe stress and
illness often are
related--and they are right.
Research has confirmed
this
belief,
showing, for instance, that
the incidence of respiratory illnesses
increases when people experience
high
levels of stress. Why is this so? One
likely answer is that stress
suppresses immune functions in
some
way,
leaving the person open to infection. The
phenomenon of stress is very important in
the
understanding
of health and wellness. We have devoted
many upcoming lectures to cover this
area.
GENETIC
PROCESSES IN DEVELOPMENT AND HEALTH
Genetic
Materials and Transmission
What
did this search yield? By the
early 20th century, researchers
discovered threadlike structures
called
chromosomes
and proposed that these
structures contained units called genes.
Soon they determined the
basic
substance common to all genetic
material-- deoxyribonucleic acid, or DNA
for short--and
described
its
structure. Today we know
that DNA determines our
growth patterns and physical
structures, We also
know
that genes are discrete
particles of DNA and that
strings of genes are
organized into
chromosomes.
The
Impact of Genetics on Development and
Health
Researchers
have determined that every
human cell contains
30.000--40,000 genes and
have identified and
mapped
almost all of the human
system of genes. Genes
control a vast number of traits,
including more
than
3,000 diseases. For some
diseases, researchers have
even pinpointed the exact
gene locations.
A
biopsychosocial perspective in our
examination of heredity is important. One way is to
study the patients
of
different diseases and find
out if they have some clues
in their lifestyles or behaviors.
For example,
disease
and genetic mutation can
result from engaging in
certain behaviors, such as
smoking cigarettes
and
eating
diets that are high in
fats and low in
fiber.
Having
this knowledge, we can also identify
other similar behaviors that
can lead to diseases, and
find ways
to
eliminate or modify them.
The
biopsychosocial perspective of heredity is
important in another way. Many
researchers believe that
we
often
inherit a predisposition or susceptibility--rather
than a certainty--for developing a
disease. This
might
account in part for the observation
that not everyone who is
exposed to harmful substances
and
microorganisms
in their environments become sick.
People who inherit a high
degree of susceptibility to a
form
of cancer and have relatively
little exposure to relevant antigens
may be just as likely to develop
the
illness
as someone who has little
genetic susceptibility but high antigen
exposure. If physicians could
determine
whether a patient has a genetic
predisposition to a specific disease, they could
provide the person
with
instructions for taking early
preventive action.
56
Table of Contents:
- INTRODUCTION TO HEALTH PSYCHOLOGY:Health and Wellness Defined
- INTRODUCTION TO HEALTH PSYCHOLOGY:Early Cultures, The Middle Ages
- INTRODUCTION TO HEALTH PSYCHOLOGY:Psychosomatic Medicine
- INTRODUCTION TO HEALTH PSYCHOLOGY:The Background to Biomedical Model
- INTRODUCTION TO HEALTH PSYCHOLOGY:THE LIFE-SPAN PERSPECTIVE
- HEALTH RELATED CAREERS:Nurses and Physician Assistants, Physical Therapists
- THE FUNCTION OF NERVOUS SYSTEM:Prologue, The Central Nervous System
- THE FUNCTION OF NERVOUS SYSTEM AND ENDOCRINE GLANDS:Other Glands
- DIGESTIVE AND RENAL SYSTEMS:THE DIGESTIVE SYSTEM, Digesting Food
- THE RESPIRATORY SYSTEM:The Heart and Blood Vessels, Blood Pressure
- BLOOD COMPOSITION:Formed Elements, Plasma, THE IMMUNE SYSTEM
- SOLDIERS OF THE IMMUNE SYSTEM:Less-Than-Optimal Defenses
- THE PHENOMENON OF STRESS:Experiencing Stress in our Lives, Primary Appraisal
- FACTORS THAT LEAD TO STRESSFUL APPRAISALS:Dimensions of Stress
- PSYCHOSOCIAL ASPECTS OF STRESS:Cognition and Stress, Emotions and Stress
- SOURCES OF STRESS:Sources in the Family, An Addition to the Family
- MEASURING STRESS:Environmental Stress, Physiological Arousal
- PSYCHOSOCIAL FACTORS THAT CAN MODIFY THE IMPACT OF STRESS ON HEALTH
- HOW STRESS AFFECTS HEALTH:Stress, Behavior and Illness, Psychoneuroimmunology
- COPING WITH STRESS:Prologue, Functions of Coping, Distancing
- REDUCING THE POTENTIAL FOR STRESS:Enhancing Social Support
- STRESS MANAGEMENT:Medication, Behavioral and Cognitive Methods
- THE PHENOMENON OF PAIN ITS NATURE AND TYPES:Perceiving Pain
- THE PHYSIOLOGY OF PAIN PERCEPTION:Phantom Limb Pain, Learning and Pain
- ASSESSING PAIN:Self-Report Methods, Behavioral Assessment Approaches
- DEALING WITH PAIN:Acute Clinical Pain, Chronic Clinical Pain
- ADJUSTING TO CHRONIC ILLNESSES:Shock, Encounter, Retreat
- THE COPING PROCESS IN PATIENTS OF CHRONIC ILLNESS:Asthma
- IMPACT OF DIFFERENT CHRONIC CONDITIONS:Psychosocial Factors in Epilepsy