 |
Abnormal
Psychology PSY404
VU
LESSON
27
MOOD
DISORDERS
Recap
Lecture No. 26
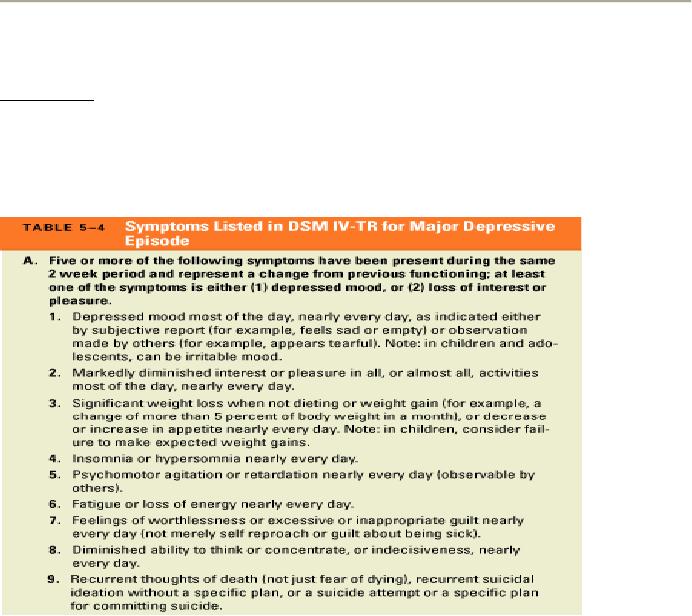
DIAGNOSIS
Unipolar
Disorders
�
The
unipolar disorders include two
specific types: major depressive disorder
and dysthymia.
�
In
order to meet the criteria for major
depressive disorder, a person must
experience at least
one
major
depressive episode in the absence of
any history of manic
episodes.
�
Dysthymia
differs
from major depression in terms of
both severity and
duration.
�
Dysthymia
represents a chronic mild depressive
condition that has been
present for many
years.
�
In
order to fulfill DSM-IV-TR criteria
for this disorder, the person must,
over a period of at least
2
years,
exhibit a depressed mood for
most of the day on more days
than not.
�
Two
or more of the following symptoms
must also be present for a
diagnosis of dysthymia:
1.
Poor appetite or
overeating
2.
Insomnia or hypersomnia
3.
Low energy or fatigue
4.
Low self-esteem
5.
Poor concentration or difficulty
making decisions
6.
Feelings of hopelessness
�
These
symptoms must not be absent
for more than 2 months at a time
during the 2-year
period.
�
If
at any time during the initial 2
years the person met criteria
for a major depressive episode,
the
diagnosis
would be major depression rather than
dysthymia.
�
As
in the case of major depressive disorder, the
presence of a manic episode
would rule out a
diagnosis
of dysthymia.
127
Abnormal
Psychology PSY404
VU
�
The
distinction between major depressive
disorder and dysthymia is somewhat
artificial because
both
sets of symptoms are
frequently seen in the same
person.
�
In
such cases, rather than
thinking of them as separate disorders,
it is more appropriate to consider
them
as two aspects of the same disorder,
which waxes and wanes
over time.
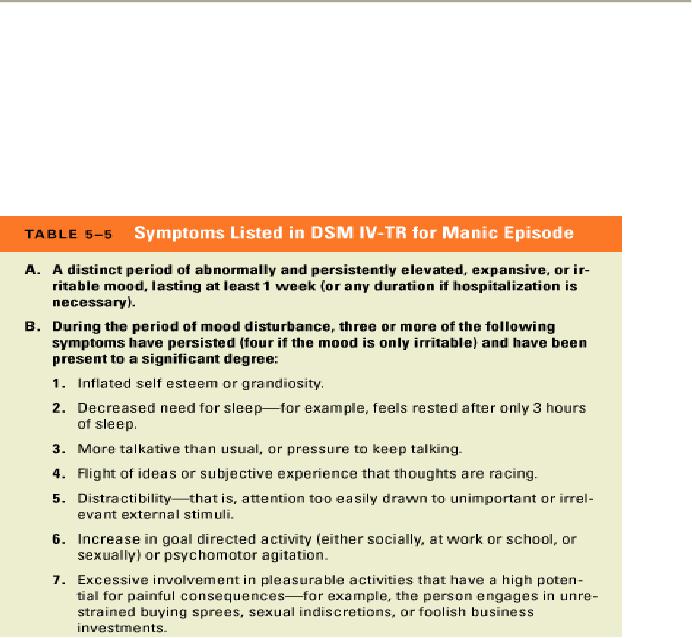
Bipolar
Disorders
�
All
three types of bipolar
disorders involve manic or hypomanic
episodes.
�
The
mood disturbance must be
severe enough to interfere with
occupational or social
functioning.
�
A
person who has experienced
at least one manic episode
would be assigned a diagnosis of
bipolar
I
disorder.
Bipolar
Disorders (continued)
�
Hypomania
refers
to episodes of increased energy
that are not sufficiently
severe to qualify as
full-
blown
mania.
�
A
person who has experienced
at least one major depressive
episode, at least one
hypomanic
episode,
and no full-blown manic
episodes would be assigned a
diagnosis of bipolar
II disorder.
�
The
differences between manic
and hypomanic episodes involve
duration and
severity.
�
The
symptoms need to be present
for a minimum of only 4 days
to meet the threshold for a
hypomanic
episode (as opposed to 1
week for a manic
episode).
�
The
mood change in a hypomanic episode
must be noticeable to others,
but the disturbance
must
not
be severe enough to impair social or
occupational functioning or to require
hospitalization.
�
Cyclothymia
is
considered by DSM-IV-TR to be a chronic
but less severe form of
bipolar
disorder.
�
In
order to meet criteria for
cyclothymia, the person must
experience numerous hypomanic
episodes
and numerous periods of
depression (or loss of
interest or pleasure) during a
period of 2
years.
128
Abnormal
Psychology PSY404
VU
�
There
must be no history of major depressive
episodes and no clear
evidence of a manic
episode
during
the first 2 years of the
disturbance.
Further
Descriptions and Subtypes
�
DSM-IV-TR
includes several additional
ways of describing subtypes of the
mood disorders.
�
These
are based on two
considerations:
1)
more specific descriptions of
symptoms that were present
during the most recent
episode
of
depression (known as episode
specifiers)
and
2)
more extensive descriptions of the
pattern that the disorder follows
over time (known as
course
specifiers).
�
One
episode specifier allows the clinician to
describe a major depressive episode as
having
melancholic
features.
�
Melancholia
is a term
that is used to describe a particularly
severe type of depression.
�
In
order to meet the DSM-IV-TR criteria
for melancholic features, a
depressed patient must
either
�
lose
the feeling of pleasure associated with
all, or almost all, activities or
�
Lose
the capacity to feel better--even
temporarily--when something good
happens.
�
The
person must also exhibit at
least three of the following to
meet the criteria of melancholia:
�
the
depressed mood feels
distinctly different from the
depression a person would feel after
the
death
of a loved one;
�
the
depression is most often worst in the
morning;
�
the
person awakens early, at
least 2 hours before
usual;
�
marked
psychomotor retardation or agitation;
�
significant
loss of appetite or weight loss;
and
�
excessive
or inappropriate guilt.
�
Another
episode specifier allows the clinician to
indicate the presence of psychotic
features--
hallucinations
or delusions--during the most recent
episode of depression or
mania.
�
Depressed
patients who exhibit
psychotic features are more
likely to require hospitalization
and
treatment
with a combination of antidepressant
and antipsychotic medication.
�
Another
episode specifier applies to
women who become depressed
or manic following
pregnancy.
�
A
major depressive or manic episode
can be specified as having a postpartum
onset if it
begins within
4
weeks after childbirth.
�
Because
the woman must meet the full
criteria for an episode of major
depression or mania, this
category
does not include minor
periods of postpartum "blues," which
are relatively common.
�
A
mood disorder (either unipolar or
bipolar) is described as following a
seasonal pattern if, over
a
period
of time, there is a regular relationship
between the onset of a person's
episodes and
particular
times of the year.
�
Researchers
refer to a mood disorder in which the
onset of episodes is regularly associated
with
changes
in seasons as seasonal
affective disorder.
�
Unipolar
Disorders
�
People
with unipolar mood disorders
typically have their first
episode in middle age; the
average
age
of onset is in the mid-forties.
�
DSM-IV-TR
sets the minimum duration at 2
weeks, but they can last
much longer.
�
In
one large-scale follow-up study, 10
percent of the patients had
depressive episodes that
lasted
more
than 2 years.
�
Most
unipolar patients will have
at least two depressive
episodes.
�
The
mean number of lifetime episodes is
five or six.
129
Abnormal
Psychology PSY404
VU
�
When
a person's symptoms are diminished or
improved, the disorder is considered to be
in
remission,
or a
period of recovery.
�
Relapse
is a
return of active symptoms in a
person who has recovered
from a previous episode.
�
Approximately
half of all unipolar
patients recover within 6 months of the
beginning of an episode.
�
The
probability that a patient
will recover from an episode
decreases after 6 months, and 10 to
20
percent
do not recover after 5
years.
�
Among
those who recover, 50 percent
relapse within 3
years.
Bipolar
Disorders
�
Onset
of bipolar mood disorders
usually occurs between the
ages of 28 and 33 years,
which is
younger
than the average age of
onset for unipolar
disorders.
�
The
first episode is just as
likely to be manic as
depressive.
�
The
average duration of a manic
episode runs between 2 and 3
months.
�
The
long-term course of bipolar
disorders is most often
episodic, and the prognosis is
mixed.
�
Most
patients have more than
one episode, and bipolar
patients tend to have more
episodes than
unipolar
patients.
�
Several
studies that have followed
bipolar patients over
periods of up to 10 years have
found that
40
to 50 percent of patients are
able to achieve a sustained
recovery from the disorder.
Incidence
and Prevalence
�
Unipolar
depression is one of the most common
forms of psychopathology.
�
Among
people who were interviewed for the
ECA study, approximately 6 percent were
suffering
from
a diagnosable mood disorder during a
period of 6 months.
�
The
ratio of unipolar to bipolar
disorders is at least
5:1.
�
Lifetime
risk for major depressive disorder was
approximately 5 percent, averaged across
sites in
the
ECA program.
�
The
lifetime risk for dysthymia
was approximately 3 percent and the
lifetime risk for bipolar
I
disorder
was close to 1
percent.
�
Almost
half the people who met
diagnostic criteria for dysthymia
had also experienced an
episode
of
major depression at some point in
their lives.
�
The
National Comorbidity Survey produced
even higher figures for the
lifetime prevalence of
mood
disorders; therefore the prevalence
estimates for mood disorders
in the ECA study are
probably
conservative.
�
Slightly
more than 30 percent of
those people in the ECA study
who met diagnostic criteria
for a
mood
disorder made contact with a
mental health professional during the 6
months prior to their
interview.
�
Gender
Differences
�
Women
are two or three times
more vulnerable to depression than
men are.
�
The
increased prevalence of depression
among women is apparently limited to
unipolar disorders.
�
Possible
explanations for this gender difference
have focused on a variety of factors,
including sex
hormones,
stressful life events, and
childhood adversity as well as
response styles that
are
associated
with gender roles.
�
Cross-Cultural
Differences
�
Comparisons
of emotional expression and
emotional disorder across cultural
boundaries encounter
a
number of methodological problems.
�
One
problem involves vocabulary.
130
Abnormal
Psychology PSY404
VU
�
Cross-cultural
differences have been
confirmed by a number of research
projects that have
examined
cultural variations in symptoms among
depressed patients in different
countries.
�
These
studies report comparable
overall frequencies of mood
disorders in various parts of
the
world,
but the specific type of symptom
expressed by the patients varies
from one culture to the
next.
�
In
Chinese patients, depression is
more likely to be described in
terms of somatic symptoms,
such
as
sleeping problems, headaches,
and loss of energy.
�
Depressed
patients in Europe and North
America are more likely to
express feelings of guilt
and
suicidal
ideas.
�
These
cross-cultural comparisons suggest that,
at its most basic level, clinical
depression is a
universal
phenomenon that is not limited to
Western or urban societies.
�
They
also indicate that a person's cultural
experiences, including linguistic,
educational, and
social
factors,
may play an important role in
shaping the manner in which he or
she expresses and
copes
with
the anguish of depression.
Risk
for Mood Disorders Across
the Life Span
�
Data
from the ECA project suggest
that mood disorders are
most frequent among young
and
middle-aged
adults.
�
Prevalence
rates for major depressive disorder
and dysthymia were significantly
lower for people
over
the age of 65.
�
The
frequency of bipolar disorders
was also low in the oldest
age groups.
�
The
frequency of depression is much higher
among certain subgroups of elderly
people.
�
The
prevalence of depression is particularly
high among those who
are about to enter
residential
care
facilities.
�
Elderly
people in nursing homes are more
likely to be depressed in comparison to a
random sample
of
elderly people living in the
community.
�
People
born after World War II seem
to be more likely to develop mood
disorders than were
people
from previous generations.
�
The
average age of onset for
clinical depression also seems to be
lower in people who were
born
more
recently; a pattern sometimes called a
birth cohort trend.
�
At
low levels and over
brief periods of time, depressed
mood may help us refocus
our motivations
and
it may help us to conserve
and redirect our energy in
response to experiences of loss
and
defeat.
�
A
disorder that is as common as depression
must have many causes rather
than one.
�
The
principle of equifinality, which holds
that there are many
ways to reach the same
outcome,
clearly
applies in the case of mood
disorders.
Social
Factors
�
The
experience of stressful life
events is associated with an
increased probability that a
person will
become
depressed.
�
Prospective
studies have found that
stressful life events are
useful in predicting the
subsequent
onset
of unipolar depression.
�
Although
many kinds of negative events
are associated with
depression, a special class
of
circumstances--those
involving major losses of important
people or roles--seem to play a crucial
role
in precipitating unipolar
depression.
�
Brown
and his colleagues believe
that depression is more
likely to occur when severe
life events are
associated
with feelings of humiliation, entrapment,
and defeat.
131
Abnormal
Psychology PSY404
VU
�
Variations
in the overall prevalence of depression
are driven in large part by
social factors that
influence
the frequency of stress in the
community.
Social
Factors and Bipolar Disorders
�
Some
studies have found that the
weeks preceding the onset of a
manic episode are marked by
an
increased
frequency of stressful life
events.
�
The
kinds of events that precede the
onset of mania tend to be
different from those that
lead to
depression.
�
While
the latter include primarily negative
experiences involving loss
and low self-esteem,
the
former
include schedule-disrupting events (such
as loss of sleep) as well as
goal attainment events.
�
Some
patients experience an increase in
manic symptoms after they have
achieved a significant goal
toward
which they had been
working.
�
Aversive
patterns of emotional expression
and communication within the family
can also have a
negative
impact on the adjustment of people with
bipolar mood
disorders.
�
Bipolar
patients who have less
social support are more
likely to relapse and
recover more slowly
than
patients with higher levels of
social support.
�
Stressful
life events can also
delay recovery from an
episode of depression in bipolar
patients.
�
The
course of bipolar mood disorder
can be influenced by the social
environment in which the
person
is living.
132
Table of Contents:
- ABNORMAL PSYCHOLOGY:PSYCHOSIS, Team approach in psychology
- WHAT IS ABNORMAL BEHAVIOR:Dysfunction, Distress, Danger
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Supernatural Model, Biological Model
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Free association, Dream analysis
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Humanistic Model, Classical Conditioning
- RESEARCH METHODS:To Read Research, To Evaluate Research, To increase marketability
- RESEARCH DESIGNS:Types of Variables, Confounding variables or extraneous
- EXPERIMENTAL REASEARCH DESIGNS:Control Groups, Placebo Control Groups
- GENETICS:Adoption Studies, Twin Studies, Sequential Design, Follow back studies
- RESEARCH ETHICS:Approval for the research project, Risk, Consent
- CAUSES OF ABNORMAL BEHAVIOR:Biological Dimensions
- THE STRUCTURE OF BRAIN:Peripheral Nervous System, Psychoanalytic Model
- CAUSES OF PSYCHOPATHOLOGY:Biomedical Model, Humanistic model
- CAUSES OF ABNORMAL BEHAVIOR ETIOLOGICAL FACTORS OF ABNORMALITY
- CLASSIFICATION AND ASSESSMENT:Reliability, Test retest, Split Half
- DIAGNOSING PSYCHOLOGICAL DISORDERS:The categorical approach, Prototypical approach
- EVALUATING SYSTEMS:Basic Issues in Assessment, Interviews
- ASSESSMENT of PERSONALITY:Advantages of MMPI-2, Intelligence Tests
- ASSESSMENT of PERSONALITY (2):Neuropsychological Tests, Biofeedback
- PSYCHOTHERAPY:Global Therapies, Individual therapy, Brief Historical Perspective
- PSYCHOTHERAPY:Problem based therapies, Gestalt therapy, Behavioral therapies
- PSYCHOTHERAPY:Ego Analysis, Psychodynamic Psychotherapy, Aversion Therapy
- PSYCHOTHERAPY:Humanistic Psychotherapy, Client-Centered Therapy, Gestalt therapy
- ANXIETY DISORDERS:THEORIES ABOUT ANXIETY DISORDERS
- ANXIETY DISORDERS:Social Phobias, Agoraphobia, Treating Phobias
- MOOD DISORDERS:Emotional Symptoms, Cognitive Symptoms, Bipolar Disorders
- MOOD DISORDERS:DIAGNOSIS, Further Descriptions and Subtypes, Social Factors
- SUICIDE:PRECIPITATING FACTORS IN SUICIDE, VIEWS ON SUICIDE
- STRESS:Stress as a Life Event, Coping, Optimism, Health Behavior
- STRESS:Psychophysiological Responses to Stress, Health Behavior
- ACUTE AND POSTTRAUMATIC STRESS DISORDERS
- DISSOCIATIVE AND SOMATOFORM DISORDERS:DISSOCIATIVE DISORDERS
- DISSOCIATIVE and SOMATOFORM DISORDERS:SOMATOFORM DISORDERS
- PERSONALITY DISORDERS:Causes of Personality Disorders, Motive
- PERSONALITY DISORDERS:Paranoid Personality, Schizoid Personality, The Diagnosis
- ALCOHOLISM AND SUBSTANCE RELATED DISORDERS:Poly Drug Use
- ALCOHOLISM AND SUBSTANCE RELATED DISORDERS:Integrated Systems
- SCHIZOPHRENIA:Prodromal Phase, Residual Phase, Negative symptoms
- SCHIZOPHRENIA:Related Psychotic Disorders, Causes of Schizophrenia
- DEMENTIA DELIRIUM AND AMNESTIC DISORDERS:DELIRIUM, Causes of Delirium
- DEMENTIA DELIRIUM AND AMNESTIC DISORDERS:Amnesia
- MENTAL RETARDATION AND DEVELOPMENTAL DISORDERS
- MENTAL RETARDATION AND DEVELOPMENTAL DISORDERS
- PSYCHOLOGICAL PROBLEMS OF CHILDHOOD:Kinds of Internalizing Disorders
- LIFE CYCLE TRANSITIONS AND ADULT DEVELOPMENT:Aging