 |
ANXIETY DISORDERS:Social Phobias, Agoraphobia, Treating Phobias |
| << ANXIETY DISORDERS:THEORIES ABOUT ANXIETY DISORDERS |
| MOOD DISORDERS:Emotional Symptoms, Cognitive Symptoms, Bipolar Disorders >> |
Abnormal
Psychology PSY404
VU
LESSON
25
ANXIETY
DISORDERS
(Symptoms
of anxiety)
(Type
of anxiety disorders)
Recap
Lecture No. 24
�
Panic
and anxiety combine to form different
anxiety disorders
�
1-
Generalized Anxiety Disorder
(GAD)
�
2-
panic with
agoraphobia
�
3-Specific
phobia
�
4-
Social phobia
�
5-Post
Traumatic Stress Disorder (PTSD)
�
6-Obessive
Compulsive Disorder (OCD)
�
Generalized
Anxiety Disorder is unfocused,
prolonged anxiety and
worry.
�
Anxiety
is about minor every day
events
�
Genetics
and psychological factors
responsible for GAD.
�
Before
GAD can be diagnosed, several criteria
must be met. According to
DSM-IV, the excessive
and
unrealistic anxiety and worry
must be present for a
minimum of six months; impulses
must be
experienced
as difficult to control; and they
must be associated with at
least three of the
following
symptoms:
�
Restlessness,
feeling on the edge
�
Easily
fatigued
�
Difficulty
in concentrating or mind going
blank
�
Irritability
�
Muscle
tension
�
Sleep
disturbance (difficulty falling or
staying asleep, or restless
and unsatisfying
sleep)
�
Although
98.6 percent of GAD patients
meet the criterion of three
out of six symptoms, a
large
percentage
of patients with other anxiety
disorders also fulfill this
criterion. Raising the criterion
to
four
or more symptoms increases
diagnostic accuracy.
Treating
GAD Borkovec
and his colleagues (1983)
have provided some interesting
information
�
about
the ability of clients to learn
how to manage their
worrying.
�
In
one study clients reported
that worry consumed approximately 50
percent of each day
and
caused
those major problems. During an
intervention, the clients participated in a program
that
included
(1) establishing a specified
half-hour period (same
place, same time) for daily
worrying, (2)
identifying
negative thoughts and task- relevant
thoughts, (3) postponing worrying
until the allotted
time,
and (4), at the time assigned
for worrying, engaging in
intense worry and problem
solving.
After
four weeks, the treated
subjects showed a reduction in the
percentage of time they spent
worrying.
�
Apparently,
providing a time and place
for worrying (stimulus
control) reduces its
detrimental
effects.
�
Phobic
disorders are tied to
specific objects or situations.
Phobias
are
intense, recurrent,
and
irrational
fears that are
disproportionate to the actual situation.
Claustrophobia,
the
fear of closed
spaces,
is a common example of a phobia.
Small room or lift
etc.
�
Most
of us have some discomfort or
fear associated with fire,
disease, snakes, and being in
small
and
enclosed places. Youngsters have
been known to avoid walking
near an abandoned
"haunted
house,"
and college students may
avoid biology courses
because they are uneasy
about the blood
that
is rumored to be a part of the lab work. To a
degree, these fears are
rational but Phobic
reactions
are irrational.
�
Phobias
involve specifiable fear
reactions --
114
Abnormal
Psychology PSY404
VU
�
Clients
with phobias recognize that
their fears are excessive
and unreasonable, and they
work to
avoid
the phobic stimulus.
�
Symptoms
such as headaches, dizziness,
stomach pains, and other
general physical complaints
are
often
reported in association with
phobias. Lack of self-confidence
and mild depression may
also
accompany
phobic conditions. Fainting has
been reported in phobic exposed to the
feared situation
or
object (such as the sight of blood),
but these reports are not as
prevalent as once thought.
�
Some
phobias, such as those
provoked by small animals,
are present in early
childhood, but phobic
disorders
typically begin in adolescence or early
adulthood.
Who
Is Affected with Phobias?
Phobic
disorders are the most common of the
anxiety disorders,
�
with
a lifetime prevalence of 14.2
percent of the population (Eaton, Dryman
& Weissman, 1991).
�
Using
current diagnostic criteria, and sampling
from more than eight
thousand people from
non-
institutional
households, Magee and
associates (1996) reported lifetime
prevalence of 13.3
percent
for
social phobia, 11.3 percent
for specific phobia, and
6.7 percent for
agoraphobia.
Specific
(Simple) Phobias
�
Specific
phobias are pathological (excessive
and unrealistic) fears of
specific animals, objects,
or
situations.
�
Common
examples include phobias of the needles,
elevators, dogs, snakes,
storms, blood,
dentists,
and
tightly enclosed spaces
although the phobic individual
may be reasonably well
adjusted when
not
directly faced by the phobic stimulus, he
or she experiences anticipatory anxiety
when aware of
an
impending situation that could force a
confrontation with the object of fear.
When the phobic
individual
is actually exposed to the phobic
stimulus, there is almost
invariably an intense
and
immediate
anxiety response.
�
For
example, the person with
needle phobia who comes in
contact with a needle will
report
sweating,
difficulty breathing, and a racing
heart. The phobic stimulus
is viewed as powerful
indeed,
as
this example illustrates. In an experiment
conducted in the Netherlands. Women with
phobias
were
shown various, slides of
phobic stimuli and given very
mild shock. The researchers
concluded
that
because phobic stimuli cause
such discomfort, they are routinely
avoided rather than faced
directly
and endured.
Social
Phobias
�
It
refers to being
asked to perform before an audience
will produce some anxiety in
almost all of us.
The
thought of having nothing to say or of
saying something inappropriate
causes us to become
self-conscious
and nervous. These are
normal, rational fears. Social
phobias, however, involve a
persistent
fear of being in a social situation in
which one is exposed to
scrutiny by others and
a
related
fear of acting in a way that
will be humiliating or embarrassing. As
self-focus increases, so
does
the anticipation of anxiety (Woody,
1996).
�
Phobic
and non-phobic individuals
have comparable concerns,
but the intensity, extremeness,
and
irrationality
of the reactions of social phobic
set them apart from their
non-phobic counterparts.
�
Examples
of social phobias include irrational
reactions to eating in public
places, using public
restrooms,
or speaking in front of large
groups of people. Like the specific
phobic, the social
phobic
experiences marked anxiety when anticipating the
phobic situation and therefore
usually
avoids
it. This avoidance
interferes with the person's daily
routine and can potentially
ruin his or
her
career.
Agoraphobia
�
The
term agoraphobia,
which
is derived from the Greek word
agora,
meaning
marketplace, was
originally
used to refer to a pathological fear of open or
public places.
�
At
present, agoraphobia is considered a
fear of being alone or of being in public
places where
escape
is difficult or where help is
not readily available in case of a
panic attack that the
person
fears
would be overwhelming. The agoraphobic
might experience intense
fear in shopping malls
115
Abnormal
Psychology PSY404
VU
during
the holidays, in crowds at concerts or
sports events, and in
tunnels, bridges, or in
public
transport.
�
Agoraphobia
also occurs within an interrelated
and overlapping cluster of
phobias, such as a
phobia
of cars, buses, planes, and
trains. As a result of agoraphobia, the
sufferer restricts travel or
requires
a companion when away from
home.
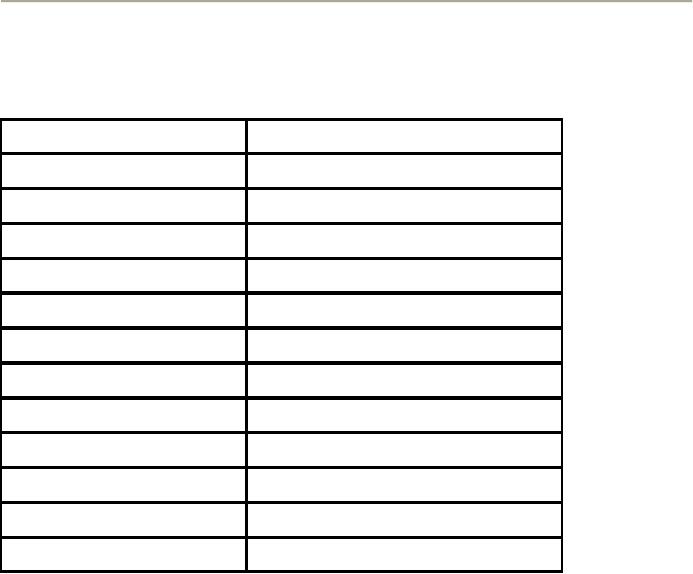
Label
Fear
Agoraphobia
Open
places
Aichmophobia
Pointed
objects
Algophobia
Pain
Arachnophobia
Spiders
Astraphobia
Storms;
thunder and lightning
Claustrophobia
Closed
spaces; confinement
Hydrophobia
Water
Nyctophobia
Darkness
Ophidiophobia
Snakes
Pyrophobia
Fire
Thanatophobia
Death
Xenophobia
Strangers
Causes
of Phobias
�
Phobic
disorders have been explained in
several ways, according to the
various models of
psychopathology.
�
For
example, the psychodynamic explanation of
phobia is that the anxiety expressed
toward the
phobic
object or situation is actually displacement of an
internal anxiety.
�
�
From
this perspective, then, a snake phobia is
more than a fear of snakes
-- it represents some
other
underlying anxiety. The phobia is
seen as having arisen because the
patient lacks
understanding
about this underlying anxiety and
uses displacement as a defense
mechanism.
�
Some
evidence of a genetic predisposition for
phobic disorder exists (Torgersen, 1983).
First,
regarding
incidence of behaviors that
are relevant to the study of social
phobia (such as eating
in
public,
being observed at work), monozygotic twins
are more alike than dizygotic twins.
Second,
parents
of children who are
diagnosed with a childhood
phobic disorder are themselves
more likely
to
meet the criteria for this disorder.
Although these findings
suggest that the pattern can
be genetic
or
learned.
�
**One
model of the development of agoraphobia specifically
includes cognitive and
behavioral
processes
�
1-
A case
of agoraphobia.
116
Abnormal
Psychology PSY404
VU
�
2-
Persons
with agoraphobia hold biased
emotional expectations; they
expect
unwanted
emotional arousal, are
overly alert to cues that
signal anxiety, and
are
highly
motivated to avoid anxiety- provoking
stimuli.
�
3-
In
persons with agoraphobia,
have an unwillingness to approach or to
try to
master
stressful situations is accompanied by a
sense of loss of
control.
Treating
Phobias
�
Specific
phobias have been
successfully treated with
systematic
desensitization,
where anxiety is
paired
with relaxation with imagined
(or real) scenes involving
the client in anxiety-producing
situations.
�
Systematic
desensitization is a behavior therapy
procedure developed by Joseph Wolpe
(1995,
1982).where
old maladaptive associations
are replaced by newer, more
adaptive ones.
�
Behavioral
exposure treatments, both
flooding and desensitization, do
provide evidence of
clients'
newly
acquired knowledge and ability to
manage anxiety. As the clients come to
experience and
accept
the ability to cope with
once-feared situations, self-efficacy
increases and remains with
the
clients
as part of their newly acquired
sense of mastery over prior
phobia.
�
To
paraphrase a familiar maxim:
Nothing succeeds like a
belief in success.
Panic
Disorder
�
The
term panic
originated
with Pan, the Greek god who
was said to be a happy but an ugly
man: He
had
the horns, ears, and legs of
a goat. When in a bad mood, he enjoyed
scaring away travelers
--
hence
the word panic
(Ley,
1987). Experiences that may
well be called panic have
been around for a
long
but it was not until
recently that consistency in
research findings and clinical
practice led to the
identification
of panic disorder as a separate type of anxiety
disorder.
�
A
person suffering from panic disorder is
vulnerable to frequent panic
attacks --
discrete
instances
of fear or discomfort. Panic attacks
are unexpected in the sense
that they do not occur
in
a
predictable context or immediately before a situation
that almost always causes
anxiety reactions;
they
are not the result of evaluation of the
person or of scrutiny by others. In these
ways, panic
disorder
is differentiated from specific
phobia and social phobia,
which do involve situational
determinants.
�
Who
Is Affected with Panic
Disorder? Panic
attacks occur in panic disorder,
but they are also
sometimes
reported in patients with
phobias, substance-abuse disorder, and
mild depression. In
one
study, researchers interviewed 1,306
residents of San Antonio,
Texas, and found that
5.6
percent
reported panic attacks, but
only 3.8 percent met
criteria for panic disorder.
�
Panic
disorder in women typically occurs at
more than twice the frequency of
panic disorder in
men.
However, research conducted in Australia
determined that, in terms of symptoms,
age of
onset,
cognition, and duration,
there are no significant differences
between male and
female
patients
with panic attacks (Oei,
Wanstall & Evans,
1990).
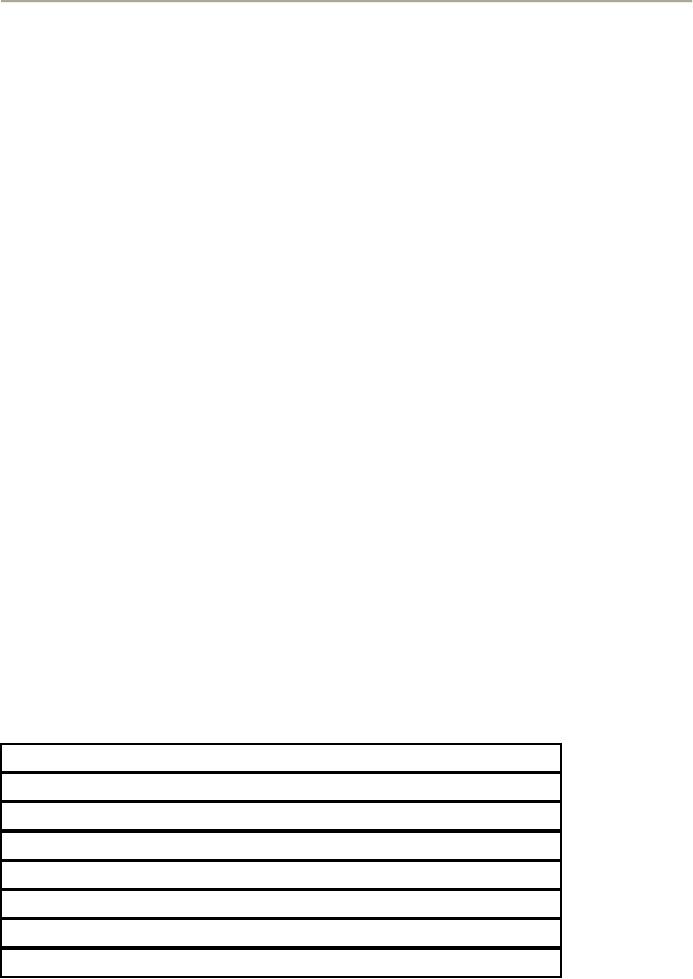
1.
Palpitations pounding heart, or
accelerated heart
rate
2.
Sweating
3.
Trembling or shaking
4.
Sensations of shortness of breath
5.
Feeling of choking
6.
Chest pain or discomfort,
7.
Nausea or abdominal distress
8.
Feeling dizzy, unsteady,
lightheaded,
117
Abnormal
Psychology PSY404
VU
9.
Derealization (feelings of unreality) or
depersonalization (feeling detached
from
oneself)
10.
Fear of losing control or going
crazy
11.
Fear of dying
12.
Numbness or tingling
sensations
13.
Chills or hot flashes
Source:
Adapted from DSM-1V Reprinted
with permission from
The
Diagnostic and
Statistical
Manual of Mental Disorders,
Fourth
Edition, Copyright @
1994
American
Psychiatric
Association.
Are
Panic Attacks
Biological?
�
**Are
panic attacks specifically
associated with biological
factors?
�
Proponents
of a biological model cite studies
showing that panic patients
responded distinctively
to
a variety of "challenges" they faced in the
laboratory. Other proponents of a
biological model
have
suggested that patients with
panic disorder have a dysfunctional
heart.
�
**panic
is a fear response to unexpected
and unexplained somatic events (Clark,
1989). It is as if
changes
in bodily functions that
can't be easily explained (such as a
sudden change in breathing)
prompt
the panic sufferer to anticipate the worst and to
experience fear and panic
(see also
McNally
& Eke, 1996).
�
According
to Clark (1986), misinterpretation of the arousal
cues is causally linked to
panic. Thus,
although
persons with panic attack
with a history of it and
those without such a history
both
experience
similar arousal (as a result
of, say, hyperventilation),
only the subjects with
panic
disorder
view these physiological cues as
indications that a catastrophe is
forthcoming. Somatic
complaints
precede the fear, and the somatic
changes are frightening to the
panic sufferer.
�
In
general, research has supported the
idea that panic attacks
result from the client's
fear response
to
certain bodily
sensations.
Obsessive-Compulsive
Disorder (OCD)
�
Have
you ever found yourself humming a
commercial jingle -- a tune that
stays in your mind
longer
than you want it to? In a small
way, this experience is like an
obsession. Obsessions
are
persistent
and unwanted thoughts, ideas, or images
that a person does not
intentionally produce.
Rather,
the unwanted thoughts are perceived as
invading the person's thinking.
The recurring
thoughts
are troublesome, unnecessary,
and distracting, and the
person tries to be rid of
them.
Features
of OCD
The
content and form of normal
and abnormal obsessions are similar.
Abnormal
obsessions,
however,
are more frequent, more intense, and of
longer duration; they produce
more
discomfort;
and they are more associated with
compulsions than are normal
obsessions.
�
Is heightened
emotional intensity possibly an important
aspect of the intrusive quality
of
obsessions?
(Clark & de Silva, 1985).
The
studies to date, using
nonclinical cases, support
this
hypothesis
and suggest that reducing
the frequency of any negative
cognition will increase
the
client's
ability to dismiss such
thoughts.
�
Although
compulsions appear to be purposeful
behaviors, they are essentially
nonfunctional and
ritualistic.
The compulsion reported most often is
checking, which results from
pathologic doubt
linked
to repeated attempts to "make
sure".
�
An
obsessive- compulsive person
might fear that the front
door was left unlocked and
so
repeatedly
return to the door to check
that it is locked. Other common examples
of compulsive
checking
include repetitions intended to determine that
gas and water taps
are shut and lights
and
118
Abnormal
Psychology PSY404
VU
appliances
are off. Still other
cases highlight a need for
organization -- checking that
kitchen
utensils
are properly aligned, cupboard
contents are correctly arranged,
and closets are organized
in
the
"right" order. Some common
rituals include repeatedly putting
clothes on and taking them
off;
hoarding
items such as newspapers, mail, or
boxes; and repeating certain
actions such as going
through
a doorway.
�
Compulsive
hand washing is linked to a preoccupation
with dirt and contamination
and may be
tinged
with reports of disgust regarding
urine and feces. Compulsive hand
washers avoid public
restrooms,
doorknobs, shaking hands,
and money, all of which are
viewed as contaminated.
Patients
may wash as many as eighty
times a day, often causing
damage to their skin.
Causes
of OCD
�
**Researchers
have speculated that the
obsessions and compulsions reflect
fixed-action patterns
that
are "wired" into the brain.
When stressful conditions
stimulate the person's perception
of
danger,
these fixed action patterns
may be inappropriately activated.
Normal individuals
cease
performing
an action when their senses tell them
that the action has been
completed, whereas,
according
to the theory just described,
persons with OCD become
helpless victims of their
repeating
patterns. Example hand
washing.
Treating
OCD
�
The
impatient friend of an obsessive
person advises, "Just don't
think about it." But the
person's
unwanted
thoughts persist nonetheless.
�
The
spouse of a compulsive checker
shouts, "We're going to be late.
Stop that damn
checking."
But
the checking continues. The
experience of nonprofessionals is that
obsessive- compulsive
disorder
is very resistant to direct instructions. Indeed,
obsessive patients have
thought and thought
about
matters that they feel are
major, and they frequently do
not respond to the suggestions
of
others.
Compulsive persons, too, are
said to be resistant to
advice.
Treatment
of OCD especially of chronic cases is
difficult earlier the treatment begins
the better it is and
when
it is becomes chronic or it goes without
any treatment for some time
then patient takes time
to
respond
to any therapy.
Posttraumatic
Stress Disorder
(PTSD)
�
Psychologically
speaking, what is similar about the
experiences of rape, torture,
military combat,
airplane
crash, earthquake, a disastrous
fire, and the collapse of a
large building? Each can
cause
severe
trauma. Posttraumatic stress disorder
(PTSD)
is a
cluster of psychological symptoms
that
can
follow a psychologically distressing
event. Stressors that
produce PTSD would produce
marked
distress
in almost anyone, and they
are outside the range of normal, common
stressors such as
chronic
illness, marital separation, or business
failure. Although not all
disasters result in
psychopathology
(Rubonis & Bickman, 1991) --
indeed, some people seem
invulnerable to the
distress
-- certain individuals do develop severe
disorders related to
trauma.
�
The
typical symptoms of PTSD occur following
a recognizable stressor (traumatic
event) that has
involved
intense fear and horror.
They include re-experiencing of the traumatic
event, persistent
avoidance
of any reminders of the event,
numbing of general responsiveness,
and increased
arousal.
To
warrant a diagnosis of PTSD, a client
must experience these
symptoms for at least one
month.
Acute
stress disorder, a recent addition to
DSM, refers to PTSD-like
reactions that persist for
at
least
two days but less
than four weeks.
**Who Is Affected with
PTSD?
According
to recent epidemiological data (Kessler
et al., 1995),
the
estimated lifetime prevalence of PTSD is
7.8 percent. The trauma
most commonly associated
with
posttraumatic
stress disorder among men is
combat exposure, which is
rated the most upsetting trauma
for
28.8
percent of men with PTSD.
Among women, rape is most
commonly associated with PTSD; it is
rated
most
upsetting by 29.9 percent of women
with PTSD. Fifty-eight percent of
battered women also
report
high
rates of PTSD (Astin, Ogland-Hand,
Coleman & Foy, 1995).
119
Abnormal
Psychology PSY404
VU
�
**Military-combat-produced
PTSD is not new; writers described
its occurrence after the Civil
War,
World
Wars I and II, and the
Korean War. Early reference
was made to "shell shock" or
"battle
fatigue"
to refer to an array of symptoms seen in
men whose military
experience included exposure
to
artillery fire, attack, and
bombings. In the United States, the
Centers for Disease
Control
conducted
a four-year epidemiological study of approximately
15,000 Vietnam veterans
and
reported
that 15 percent suffered
from combat-related PTSD since
their discharge (Roberts,
1988).
Catastrophes
such as aircraft disasters, tornadoes,
and fires can also
produce widespread and
serious
emotional
problems. An aircraft crash at a major
airport can cause emotional
stress reactions in any of
the
surviving
passengers or flight crew as
well as in witnesses to the crash, in
members of the families or
work
associates
waiting for passengers to arrive,
and in the airport employees
who are asked to assist in
the
emergency
services and crash cleanup.
Only some of those involved
actually suffer diagnosed PTSD or
acute
stress disorder, but case
reports nevertheless indicate widespread
distress. After mobilizing
energies
and
working cooperatively during the
immediate time of the emergency, people
soon tire. When the
event
has
passed and is no longer the topic of
conversation, people report loss of
sleep, a reliving of the
experience,
and fearful dreams.
**Treating PTSD
�
The
psychological treatment of clients with
posttraumatic stress disorder has
generated interest and
enthusiasm.
The research literature is young, however,
because PTSD did not appear
as an
identifiable
form of disorder until 1980. An
early and practical first
step was Operation Outreach,
a
program
designed specifically for
Vietnam combat veterans. At
Operation Outreach, any
veteran
can
find a needed outlet for
his or her emotional
distress.
�
**An
approach has proved effective in the
management of PTSD among rape
victims. Edna Foa
and
her colleagues (1991) reported
that a cognitive-behavioral treatment and a
prolonged exposure
treatment
(at follow-up) were more
effective in reducing PTSD
symptoms.
�
Many
of the rape victims who were
offered treatment declined to participate. This
may be related
to
rape victims' tendency to avoid
confrontation of the rape memory, a
tendency that is
symptomatic
of PTSD. In addition, some rape victims
may not show symptoms of
any disorder or
may
not see themselves as
patients in need of treatment.
Nevertheless, cognitive-behavioral
and
exposure
treatments seem to be helpful to PTSD
sufferers, whether veterans or rape
victims.
CLASSIFYING
AND TREATING ANXIETY
DISORDERS
"Neuroses
Are No Longer a Psychological
Problem!" If such a headline
had appeared in the
newspaper,
it would have been technically
accurate, because, the DSM IV TR
system abandoned the
use
of terms and categories
related with neurosis. For
example, phobic neurosis is
now called specific
phobia
or social phobia, and
obsessive-compulsive neurosis became
obsessive- compulsive disorder.
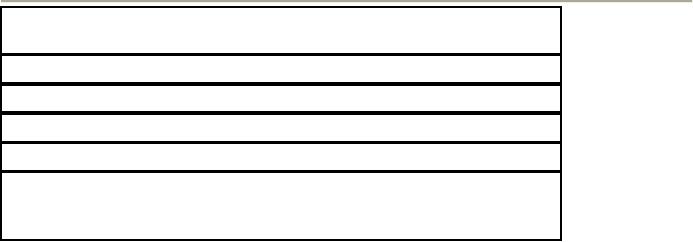
Panic
and anxiety combine to form different
anxiety disorders
1-
Generalized Anxiety Disorder
(GAD)
2-
Panic with
agoraphobia
3-
Specific phobia
4-
Social phobia
5-
Post Traumatic Stress Disorder
(PTSD)
6-
Obsessive Compulsive Disorder
(OCD)
�
Anxiety
is very hard to study. In humans a sense of
uneasiness, looking worried
and anxious.
�
The
physiological response of anxiety is reflected in
increased heart beat and
muscle tension.
�
Anxiety
is not pleasant; it is some
unpleasant thing most commonly
observed.
120
Table of Contents:
- ABNORMAL PSYCHOLOGY:PSYCHOSIS, Team approach in psychology
- WHAT IS ABNORMAL BEHAVIOR:Dysfunction, Distress, Danger
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Supernatural Model, Biological Model
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Free association, Dream analysis
- PSYCHOPATHOLOGY IN HISTORICAL CONTEXT:Humanistic Model, Classical Conditioning
- RESEARCH METHODS:To Read Research, To Evaluate Research, To increase marketability
- RESEARCH DESIGNS:Types of Variables, Confounding variables or extraneous
- EXPERIMENTAL REASEARCH DESIGNS:Control Groups, Placebo Control Groups
- GENETICS:Adoption Studies, Twin Studies, Sequential Design, Follow back studies
- RESEARCH ETHICS:Approval for the research project, Risk, Consent
- CAUSES OF ABNORMAL BEHAVIOR:Biological Dimensions
- THE STRUCTURE OF BRAIN:Peripheral Nervous System, Psychoanalytic Model
- CAUSES OF PSYCHOPATHOLOGY:Biomedical Model, Humanistic model
- CAUSES OF ABNORMAL BEHAVIOR ETIOLOGICAL FACTORS OF ABNORMALITY
- CLASSIFICATION AND ASSESSMENT:Reliability, Test retest, Split Half
- DIAGNOSING PSYCHOLOGICAL DISORDERS:The categorical approach, Prototypical approach
- EVALUATING SYSTEMS:Basic Issues in Assessment, Interviews
- ASSESSMENT of PERSONALITY:Advantages of MMPI-2, Intelligence Tests
- ASSESSMENT of PERSONALITY (2):Neuropsychological Tests, Biofeedback
- PSYCHOTHERAPY:Global Therapies, Individual therapy, Brief Historical Perspective
- PSYCHOTHERAPY:Problem based therapies, Gestalt therapy, Behavioral therapies
- PSYCHOTHERAPY:Ego Analysis, Psychodynamic Psychotherapy, Aversion Therapy
- PSYCHOTHERAPY:Humanistic Psychotherapy, Client-Centered Therapy, Gestalt therapy
- ANXIETY DISORDERS:THEORIES ABOUT ANXIETY DISORDERS
- ANXIETY DISORDERS:Social Phobias, Agoraphobia, Treating Phobias
- MOOD DISORDERS:Emotional Symptoms, Cognitive Symptoms, Bipolar Disorders
- MOOD DISORDERS:DIAGNOSIS, Further Descriptions and Subtypes, Social Factors
- SUICIDE:PRECIPITATING FACTORS IN SUICIDE, VIEWS ON SUICIDE
- STRESS:Stress as a Life Event, Coping, Optimism, Health Behavior
- STRESS:Psychophysiological Responses to Stress, Health Behavior
- ACUTE AND POSTTRAUMATIC STRESS DISORDERS
- DISSOCIATIVE AND SOMATOFORM DISORDERS:DISSOCIATIVE DISORDERS
- DISSOCIATIVE and SOMATOFORM DISORDERS:SOMATOFORM DISORDERS
- PERSONALITY DISORDERS:Causes of Personality Disorders, Motive
- PERSONALITY DISORDERS:Paranoid Personality, Schizoid Personality, The Diagnosis
- ALCOHOLISM AND SUBSTANCE RELATED DISORDERS:Poly Drug Use
- ALCOHOLISM AND SUBSTANCE RELATED DISORDERS:Integrated Systems
- SCHIZOPHRENIA:Prodromal Phase, Residual Phase, Negative symptoms
- SCHIZOPHRENIA:Related Psychotic Disorders, Causes of Schizophrenia
- DEMENTIA DELIRIUM AND AMNESTIC DISORDERS:DELIRIUM, Causes of Delirium
- DEMENTIA DELIRIUM AND AMNESTIC DISORDERS:Amnesia
- MENTAL RETARDATION AND DEVELOPMENTAL DISORDERS
- MENTAL RETARDATION AND DEVELOPMENTAL DISORDERS
- PSYCHOLOGICAL PROBLEMS OF CHILDHOOD:Kinds of Internalizing Disorders
- LIFE CYCLE TRANSITIONS AND ADULT DEVELOPMENT:Aging